Managing a patient’s pain can be difficult because pain is an intensely personal experience that cannot be measured objectively
Pain is invaluable, although we may not appreciate it at the time; it warns us of actual or impending tissue damage and strongly motivates us to take protective action. Everyone has suffered pain, the cruel persistence of a headache, a cut finger, an injured toe, or a burn wound.
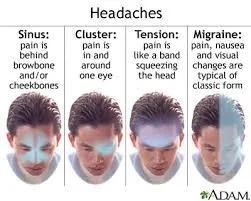
Image credit
Pain is a complex, subjective experience and may or may not be verbalized; the agency for Healthcare Research and Quality (AHRQ) reports that the most reliable indicator of the existence and intensity of pain is the patient’s self-report. Pain produces many harmful effects that inhibit healing and recovery from critical illness.
The International Society for the study of Pain, defined pain as:
“An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.”
McCaffery provides an operational definition of pain that considers the subjectivity and individuality of the pain experience and is based on the premise that the individual experiencing the pain is the true authority:
“Pain is whatever the experiencing person says it is, existing whenever he or she says it does.”
Pain management has become a national priority in recent years, yet pain continues to be misunderstood, undertreated and poorly assessed in many healthcare settings. To be able to achieve effective pain control, nurses need a clear understanding of concepts related to pain assessment and management. Uncontrolled pain causes the triggering of physical and emotional stress responses, increases the risk of other complications, inhibits healing and increases the length of hospital stay.
Pain receptors are activated by extremes of pressure and temperature as well as a veritable soup of chemicals released from injured tissue. Sensory receptors are specialized to respond to changes in their environment, which are called stimuli. Activation of a sensory receptor by an adequate stimulus results in graded potentials that in turn trigger nerve impulses along the afferent Peripheral nervous system (PNS) fibers coursing to the Central nervous system (CNS). Sensory receptors classify general sensory receptors by structure, stimulus detected and body location.
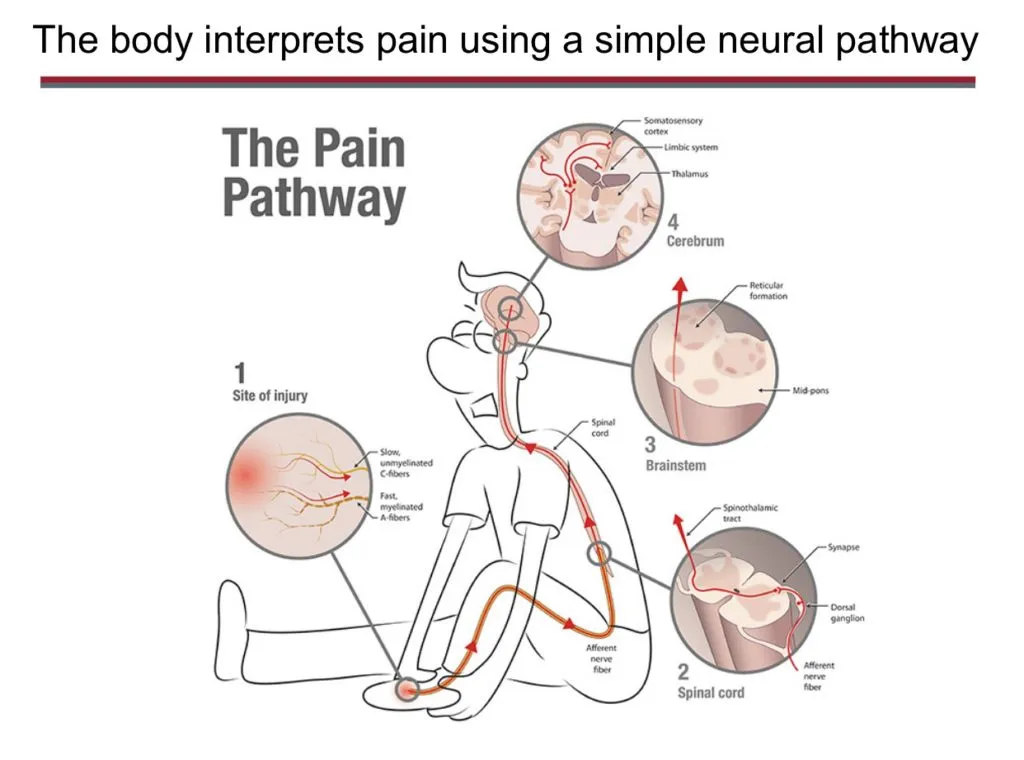
Image credit
TYPES OF PAIN
The three basic categories of pain generally recognized
- Acute pain
- Chronic pain
- Cancer-related pain
1. ACUTE PAIN
Acute pain is a protective mechanism that alerts the individual to a condition or experience that is immediately harmful to the body. The onset of acute pain is usually sudden and the pain is relieved after the chemical mediators that stimulate the nociceptors are removed. Acute anxiety is always associated with acute pain.
Acute pain is associated with a specific injury and indicates that damage or injury has occurred. Pain is significant in that it draws attention to its existence and teaches the person to avoid similar potentially painful situations. If no lasting damage occurs and no systemic disease exists, acute pain usually decreases along with healing, normally in less than six months and usually less than one month. Acute pain can be described as lasting from seconds to six months.

image credit
Acute pain caused by injuries or disease, may require treatment or may heal spontaneously. A fracture requires treatment and the pain decreases in time as the bone and injured tissue heals. A small cut on the finger heals rapidly with the pain subsiding quickly and no treatment is required.

Image credit
To follow
Part 2: Chronic pain
If you find this useful and interesting,
Look out for part 2 next week Friday
@frieda
resteem, upvote, follow