In part one of this topic, I talked about the need for renal replacement therapy(RRT) in patients with End Stage Renal Disease and the dialysis option in detail.
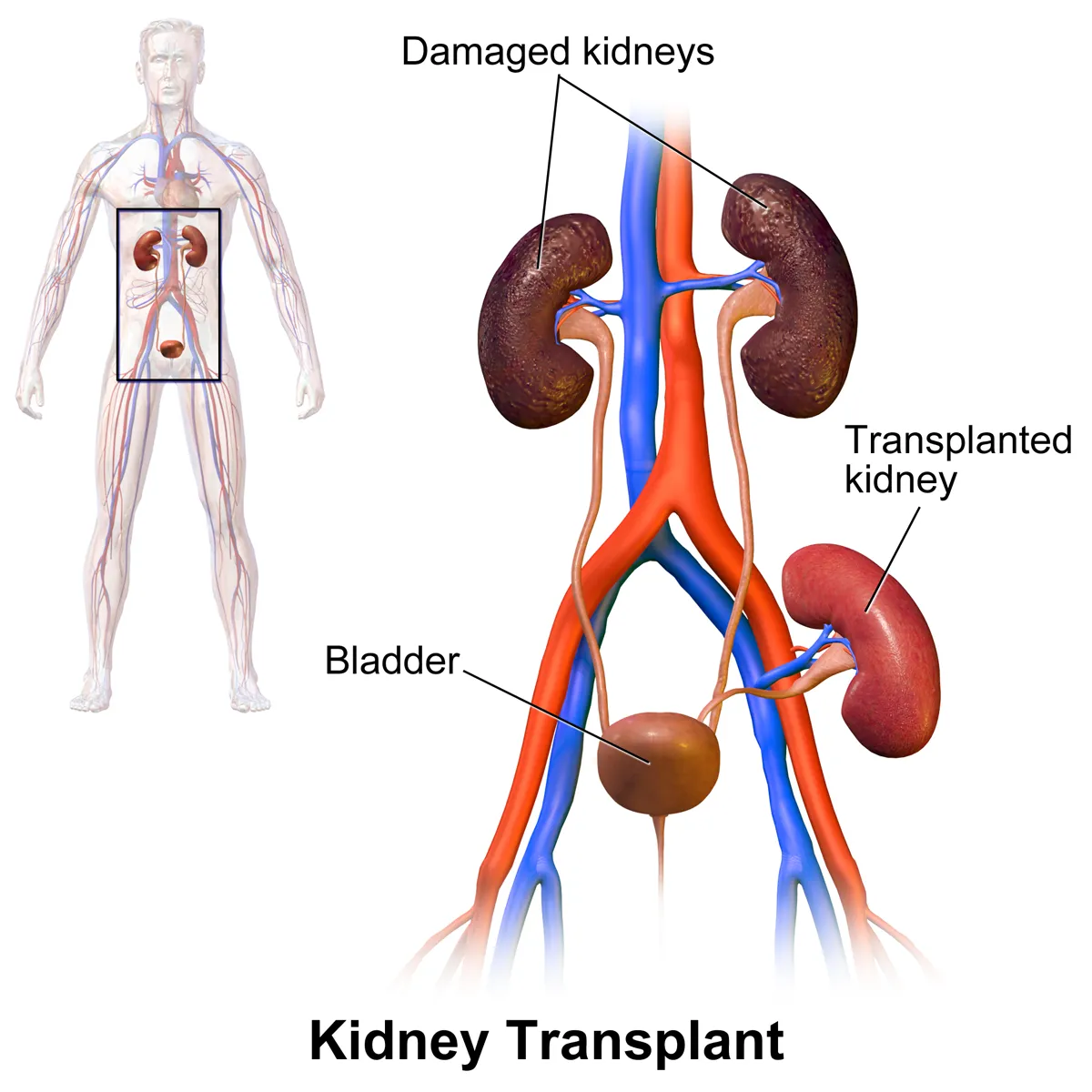
By BruceBlaus - Own work, CC BY-SA 4.0, Wikimedia
KIDNEY TRANSPLANT
This is the treatment of choice for patients with End Stage Renal Disease or advanced kidney disease. However, due to a paucity of funds, many patients cannot afford this and rely on the dialysis option. In this procedure, a healthy kidney from the donor is used to replace the diseased kidney in the recipient.
The donor here can be a living donor or a non-living donor. The living donor can be related or unrelated to the recipient and always have a better outcome. While the non-living donor can be a donor after cardiac death (DCD) or donor after brain stem death (DBD) and has a higher risk of adverse outcomes.
BEFORE THE TRANSPLANT
Before the kidney is transplanted, there is always a pre-transplant workup done for both the donor and the recipient. In this workup, they are both screened properly. A virology test is usually done to check for HIV, Hepatitis, Cytomegalovirus, etc. This is to avoid the infection of the recipient and also for the safety of those performing the procedure. An immunology test is also done to check the blood groups and rhesus antibodies to ensure compatibility.
A hematology test is done to check the full blood count, coagulation profile, thrombophilia screen, etc. This is to avoid excessive bleeding and hypovolemic shock during the process. Other tests may include chest x-ray, Electrocardiogram, carotid artery doppler, etc. For the female donor, in addition to these, a pap smear and mammogram are also done.
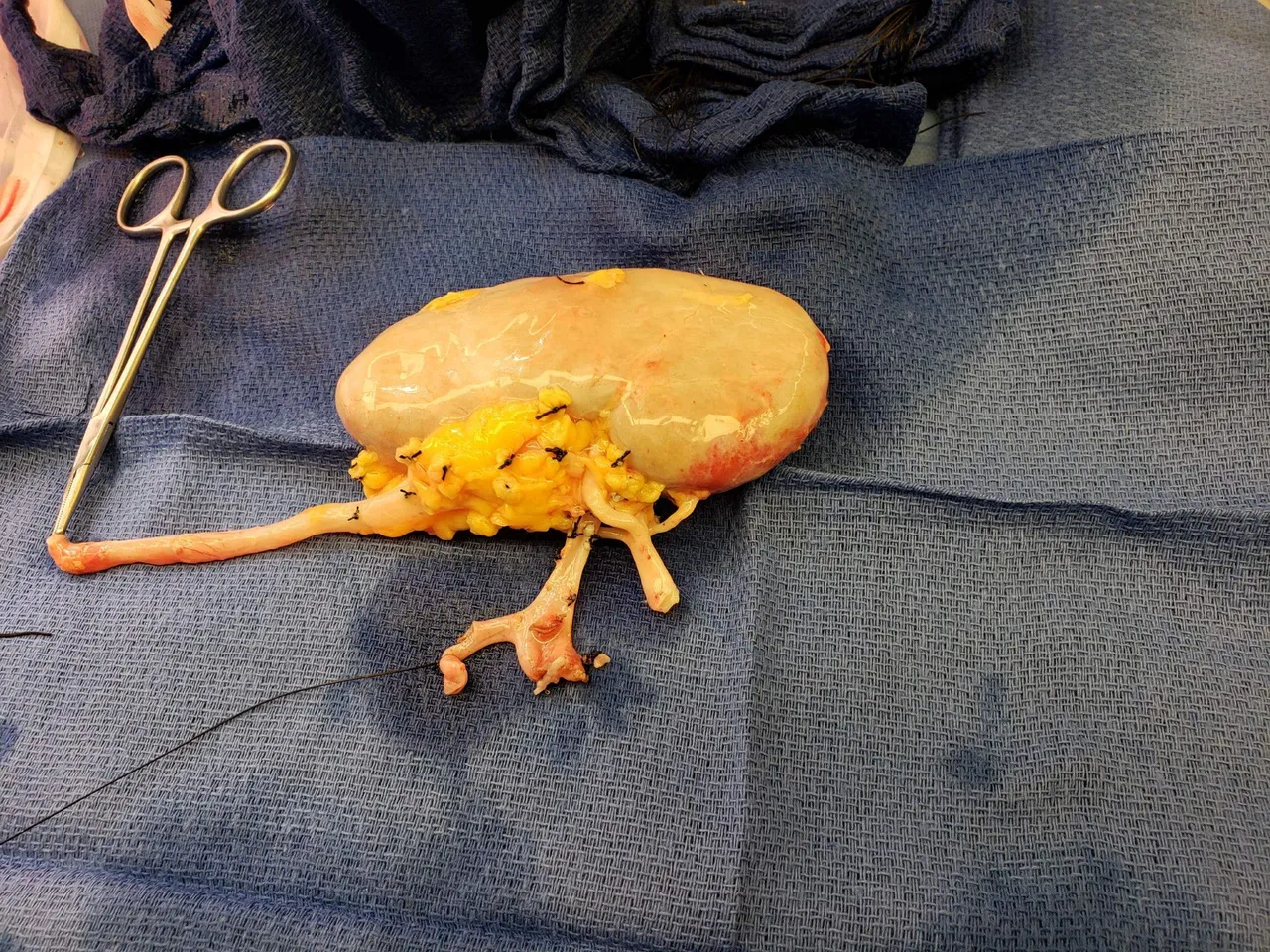
By Rmarlin - Own work, CC BY-SA 4.0, Wikimedia
DURING THE TRANSPLANT
During the operation, the healthy kidney is usually put in the right lower part of the abdomen called the right iliac fossa, and then connected with the renal vessels of the recipient. Other details of the surgery are beyond the scope of this discussion.
AFTER THE TRANSPLANT
Postoperatively, what to look out for especially is the urine output for both the donor and the recipient to ensure that they are both making urine. This gives the assurance that the kidneys are functioning. We also check if there is any bleeding or blood in the urine.
The recipient is then placed on immunosuppressants for life. Immunosuppressants are drugs that help to reduce a person's immunity. This drug is given because the body recognizes the new kidney as a foreign body and will activate the body's immune system to fight and destroy it. But with drugs to suppress the immune system, this action will be greatly reduced.

By SSgt. Derrick C. Goode - Public Domain, Wikimedia
The immunosuppressants are usually given in two phases; induction therapy and maintenance therapy.
For the induction therapy, a monoclonal anti-C25 antibody like basiliximab is given for 2 weeks. Then for the maintenance therapy, a triple regimen is given. These are 1. Prednisolone 2. Calcineuric inhibitors like Tacrolimus 3. Antimetabolite like Azathioprine.
THE FUTURE
The existing renal replacement options are faced with their peculiar challenges. Those who go for dialysis face the challenge of having to get dialyzed multiple times in a week (about 3 times), in addition to the associated cost per session. Kidney transplant on the other hand too has their challenges. The high cost of the procedure and the unavailability of the donor kidneys. They will also have to be on immunosuppressants for life.
Scientists have continued to search for better ways to improve the quality of life of these patients as well as save costs. This has led to various kinds of research ongoing, which include;
- The bioartificial or implantable kidney,
- The Laboratory-grown living kidneys, and
- The wearable (or portable) artificial kidney.
A great breakthrough in this journey is The kidney project, by a team of researchers at the University of California. They developed a bioartificial kidney which will be transplanted similarly to the donor kidney transplant that is done now. But the good side of this project is that the cells will be bioengineered from the patient's own cells, so the body won't see it as a foreign body and attack it, as it does in the donor kidney transplant. So the patient here won't have to be on immunosuppressants for life. This will greatly improve the patient's quality of life by removing the side effects associated with the long use of immunosuppressants.
A bioartificial kidney is being developed that consists of a blood filtration unit (called the hemofilter) and human kidney cells (called the bioreactor). The live cells could theoretically perform other important functions of a real kidney, such as releasing hormones to control blood pressure.
The clinical trial of this great innovation is billed to commence this year, 2022.

By Katzze.fritz - Own work, CC BY-SA 4.0, Wikimedia
Another novel research that is still in its early days is the development of laboratory-grown living kidneys. This research is focused on using stem cells or cloned tissues to grow a complete human kidney. This will also solve the problem of transplant rejection and the long use of immunosuppressants since the kidney is grown from the patient's own cells.
A team from Manchester University is the first in the world to have grown the parts of the kidney that filter blood (nephrons) in a laboratory dish using human stem cells. The laboratory-grown nephrons were then implanted into a mouse. They were able to filter the animal’s blood and produce urine, similar to how a normal kidney works.
And the third on this list is the portable artificial kidney which will be a great improvement on the existing dialysis methods. It will also be more convenient and efficient to use, with improved quality of life.
These backpack-sized dialysis devices could potentially allow a person to do blood-filtering dialysis (hemodialysis) at any time and any place. This would mean more frequent removal of waste and fluid and the ability to do dialysis ‘on the go' or away from home. This could improve people’s quality of life
The clinical trials are also billed to commence between 2022 and 2023.
Two of the best-known lightweight dialysis devices in development are:
The Ambulatory Kidney to Improve Vitality (AKTIV), was developed at the University of Washington, USA.
The Neokidney was developed by the Dutch Kidney Foundation in partnership with several companies.
When the clinical trials are successfully completed and finally approved by FDA for commercial use, these novel inventions will be game changers in the management of patients with End Stage Renal Disease. There will be a great improvement in the quality of life, less costs, and an overall better outcome.
Thanks for reading till the end.
For references and further reading;