Today I want to talk about a challenge faced by over 75 million people worldwide who have Chronic Kidney Disease. In this condition, the kidney functions decline and the rate at which the kidney filters the blood reduces progressively. To measure kidney function, we use the glomerular filtration rate, which is an assessment of how well the kidney can filter the waste products and toxins from the blood.
For a normal functioning kidney, the glomerular filtration rate (eGFR) ranges from 90 - 120ml/min/1.73m². However, when this eGFR value declines to below 15ml/min/1.73m², the patient is said to have an end-stage renal disease (ESRD). At this stage, the treatment of choice is renal replacement therapy (RRT).
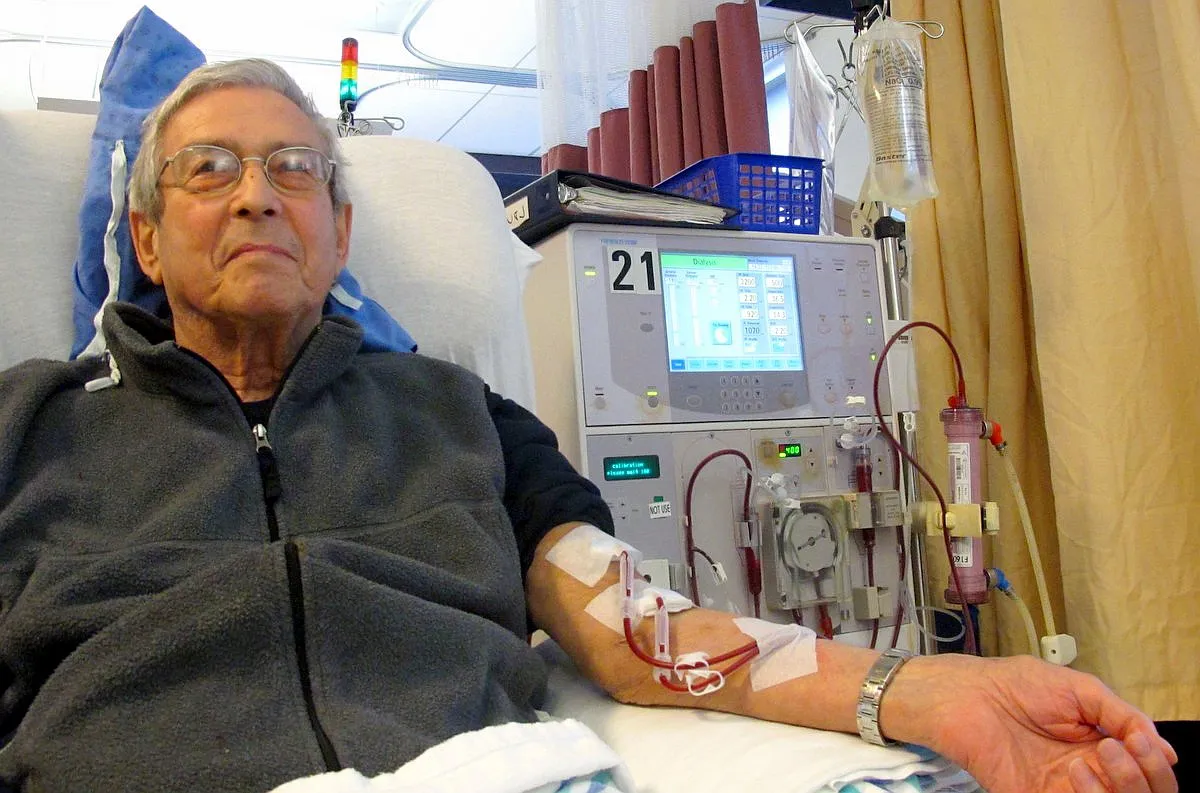
By Anna Frodesiak - Own work, CC0, Wikimedia
This procedure has saved many lives and helped to improve the quality of life in patients with End Stage Renal Disease. However, the procedures are associated with some peculiar challenges.
There are two available options for renal replacement therapy which are Dialysis and Kidney transplant. This topic is a very broad one, so I will divide it into two parts. In this part, I will talk about hemodialysis and peritoneal dialysis, then in part two, I will talk about kidney transplants and the new inventions which will be the future of renal replacement therapy.
But before we go into the details, let's briefly talk about kidney functions and the effects when the kidney cannot carry out these functions.
THE EFFECTS OF KIDNEY DISEASE
The major function of the kidney is to filter blood. The kidneys filter the waste products and toxins from the blood so that they will not accumulate in the body and cause problems. In chronic kidney disease, the function of the kidneys is greatly impaired, and therefore waste and toxic substances accumulate in the blood. Some of these toxic substances include urea, creatinine, etc.

By BAXTER CZECH - CC BY-SA 3.0, Wikimedia
Urea in particular is very toxic to the body. When urea accumulates in the blood and is carried to the brain, it affects the brain and results in what is called uremic encephalopathy. The patient develops seizures, flapping tremors, confusion, altered sleep pattern, etc. At this point, the patient has to be placed on dialysis immediately.
Accumulated urea also causes uremic gastritis which is evidenced by protracted vomiting, stomach pain, vomiting of blood, etc. Excessive urea in the blood can also affect the covering of the heart, and cause uremic pericarditis which manifests with chest pain. When urea accumulates in the skin, it causes uremic frost and itching. These are all indications for dialysis. So you can see that the kidney is a very important organ in the body. When it functions normally, it filters urea out of the blood and we won't see all these problems.
The kidney also helps in fluid and electrolyte balance, that's why kidney problems result in fluid accumulation in the body. There can also be a reduction in urine output. When the urine output becomes less than 400ml/day, and also when there is an edema that is not responding to diuretics, dialysis becomes the next option.
The kidney also produces the hormones called erythropoietin which helps in red blood cell production. So renal disease will impair red blood cell production and cause anemia. The kidney also regulates blood pressure and kidney disease is a major cause of hypertension globally.

By Irvin calicut - Own work, CC BY-SA 3.0, Wikimedia
So, what dialysis does is take over the filtration functions of the kidney. During dialysis, the patient's blood is passed through a filter which helps to filter out the waste products. However, it does not perform other functions of the kidneys like the production of Erythropoietin. There are two types of dialysis; Haemodialysis and Peritoneal dialysis. Let's look at the differences, advantages, and disadvantages of the two.
HEMODIALYSIS
The first type of dialysis is hemodialysis. In hemodialysis, the blood leaves the patient and is filtered in a dialyzer which acts as the artificial kidney. It has the dialysate and the dialysis membrane. Before the dialysis is done, vascular access is usually secured which can either be permanent access or temporary access. Vascular access is a route to get into the patient's blood vessel to enable the blood to be passed through the dialysis machine for filtration. In our facility here, we commonly use temporary access. But let me briefly talk about permanent access.
The permanent vascular access is usually the atrial ventricular fistula (AV fistula) where the vascular surgeon creates an anastomosis between the brachial artery and the cephalic vein. The anastomosis is then allowed to mature for about 6-8 weeks after which it can be used for dialysis. This is the best form of vascular access for dialysis.
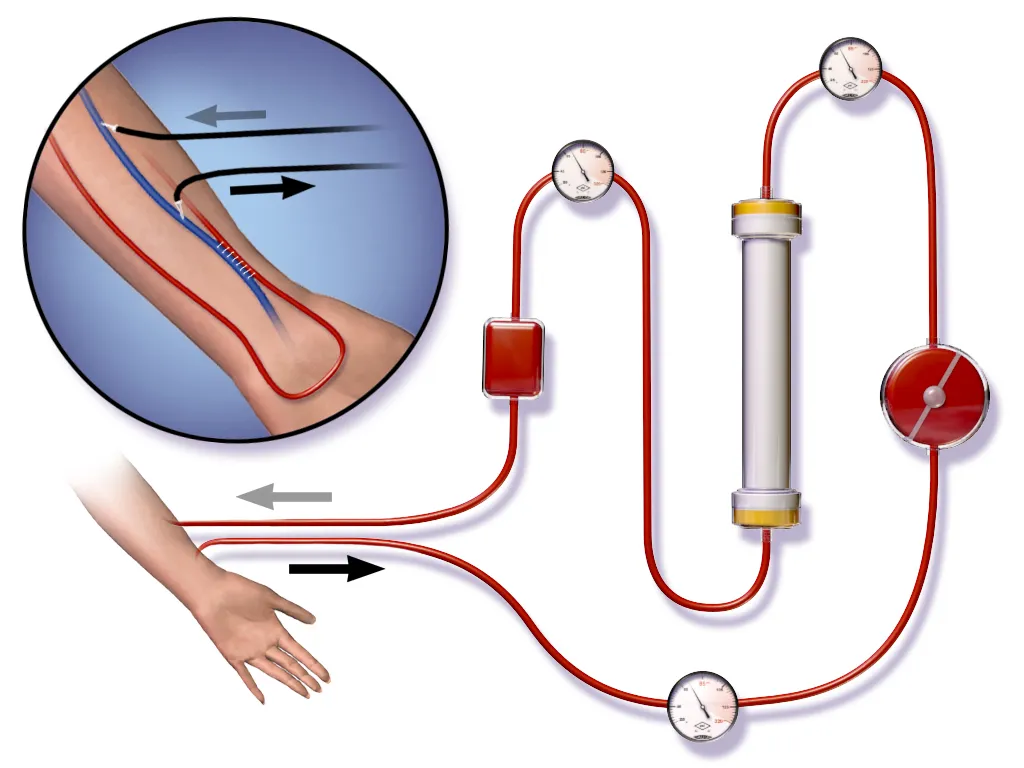
By BruceBlaus - Own work, CC BY 3.0, Wikimedia
The second form of permanent vascular access is the poly tetra fluoro ethynyl (PTFE) graft. Here, a graft is placed between an artery and a vein. This is mostly done for diabetic patients because they usually have poor vascular access. It can also be done where there is difficult anastomosis of the vessels.
For the temporary access, we either do a tunneled line or femoral access. For the tunneled line, a catheter is placed into either the internal jugular vein or the subclavian vein using the tunneled catheter. This can be used for 1 - 3 months and then it's changed. For femoral access, a femoral catheter is placed in the femoral vein and it is removed after each procedure.
Dialysis is usually done for 3 hours for first-timers and then for 4 hours per session in subsequent visits. Those with Chronic Kidney Disease, are put on maintenance hemodialysis 3 times a week for life. But for those with Acute Kidney Injury, Dialysis is usually done on alternate days and within 3-6 weeks, the kidney is expected to have recovered.
INDICATIONS FOR DIALYSIS
In addition to the clinical indications for dialysis that I mentioned above which includes uremic encephalopathy, uremic pericarditis, uremic gastritis, oliguria, acute pulmonary edema, refractory edema, etc there are also laboratory indications for dialysis. When there are elevated levels of Serum potassium, bicarbonate, urea, and creatinine above some cut-off marks, dialysis is also recommended.

By Alirezarezai99 - Own work, CC BY-SA 4.0, Wikimedia
COMPLICATIONS OF HEMODIALYSIS
There are some complications of hemodialysis of which intradialytic hypotension is the commonest. This can happen either when a patient takes an antihypertensive drug on the morning of the dialysis or when the dialysis procedure is done at a high flow rate. The normal standard flow rate for hemodialysis is 250-350 ml/min. When there is a higher flow rate and the blood leaves the patient at that high rate, it drops the blood pressure abruptly and leads to hypotension.
Another complication of hemodialysis which we experience mostly in first timers is dialysis disequilibrium syndrome (DDS). This is because those going through dialysis for the first time still have an elevated urea level which is an osmotically active molecule. When this is filtered during dialysis, it causes an osmotic shift within the blood-brain barrier. This causes the patient to develop some symptoms of encephalopathy. When noticed, the dialysis is stopped and the patient is properly resuscitated.
Other complications of hemodialysis include infection through the vascular site, formation of blood clots (thrombus), bleeding, headache, air embolism, cardiovascular disease, etc.
PERITONEAL DIALYSIS
The second type of dialysis is Peritoneal Dialysis. In peritoneal dialysis (PD), a catheter is passed through the umbilicus into the peritoneal cavity. The catheter commonly used here is the Tenckhoff catheter. Then a dialysis solution is instilled into the peritoneal cavity where blood is then filtered across the peritoneum which serves as a semi-permeable membrane.
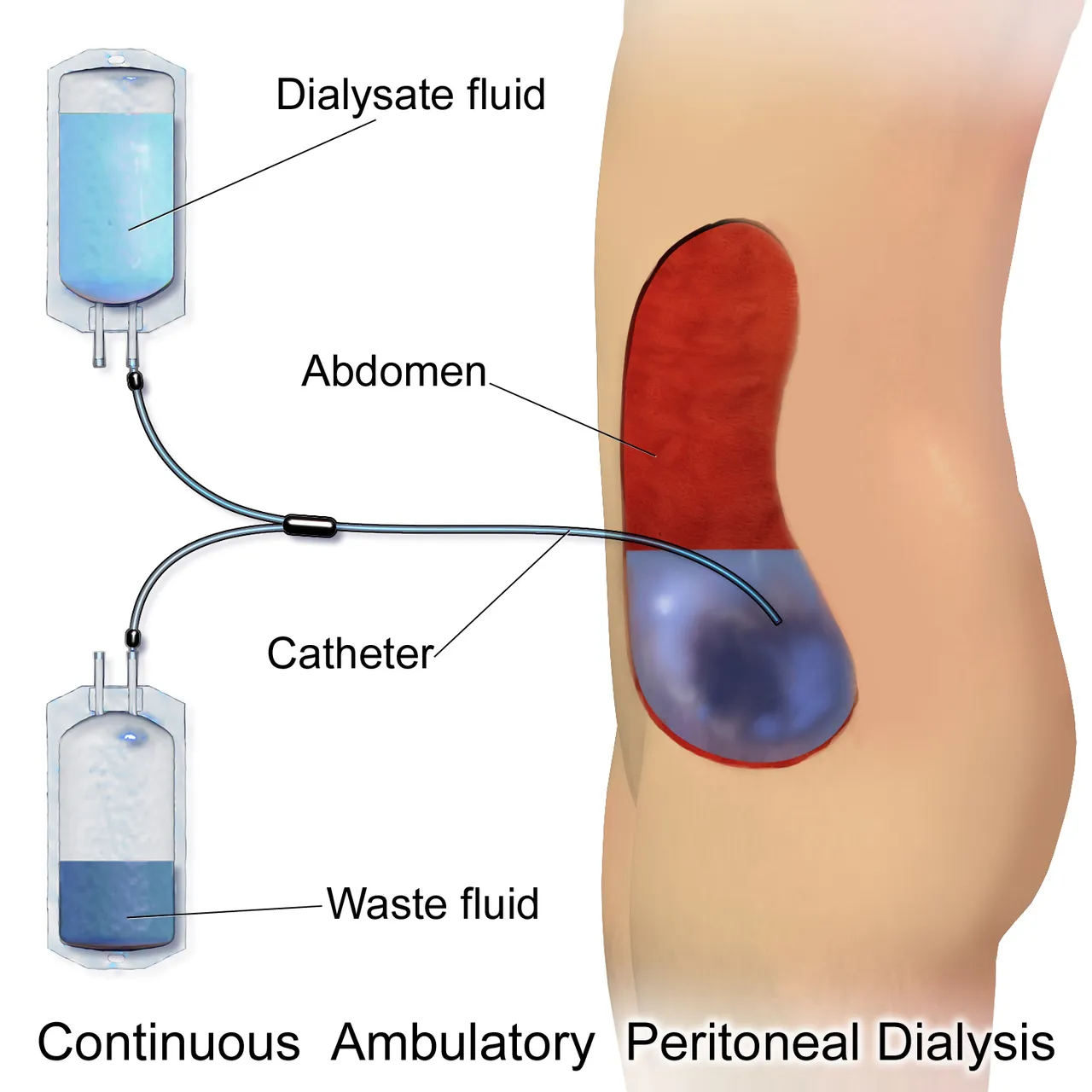
By BruceBlaus - Own work, CC BY 3.0, Wikimedia
Here, there is an exchange of water and solutes between the capillary blood and the dialysate in the peritoneum. This has two valves, one valve takes the fluid into the peritoneum while the other serves as the exit. This helps to filter out all the accumulated waste products that are causing the problem for the patient.
The advantage of this peritoneal dialysis over hemodialysis is that it's actually cheaper, more convenient, and more tolerated by most patients. It is very simple to perform and can even be done at home. The patient won't need to come to the hospital before it's done. It does not also need any of the vascular access I listed above in the hemodialysis. So there is a lesser chance of introducing microorganisms into the blood (sepsis).
However, it is a continuous therapy, and patients and relatives can get tired at some point. The failure rate of the technique is also high.
Peritoneal dialysis is of two main types;
Continuous ambulatory peritoneal dialysis (CAPD) which is usually done manually. Here, the patient instills a certain amount of dialysis fluid in the abdomen, leaving it for sometimes to allow filtration to take place and then drain it out. This helps to filter the waste products in the blood and is usually done about 4-5 times daily.
The Automated Peritoneal Dialysis (APD) which uses a machine for the fluid exchange, unlike the CAPD which is done manually. The machine does the exchange here at night when the patient is asleep. It can also be done during day time.
The commonest complication of peritoneal dialysis is the inflammation of the peritoneal membrane (peritonitis) which results from contamination of the peritoneum by skin bacteria. Other complications include infection of the catheter exit site, drainage problems, etc. So relatively, they have milder complications compared to hemodialysis.
Even though most clinicians are of the opinion that peritoneal dialysis is a better option than hemodialysis, the choice of which method to use for a particular patient depends on the patient's preference as well as the clinical state.
In the second part of this topic, we will look at the kidney transplant and the novel procedures under clinical trial which will be a game changer in the management of kidney diseases. Please stay tuned.
For references and further reading: