
An alternative perspective on mental health and addiction.
Contents
Forward
What if Doctor is Wrong? : The Research and Practices
Chapter One: Basic Instinct
Chapter 2: The Importance of Words (Part 1
Chapter 2: The Importance of Words (Part 2)
Chapter 2: Citations, Bibliography and additional sources
Chapter 3: But I Don't Have Trauma

Words are important.
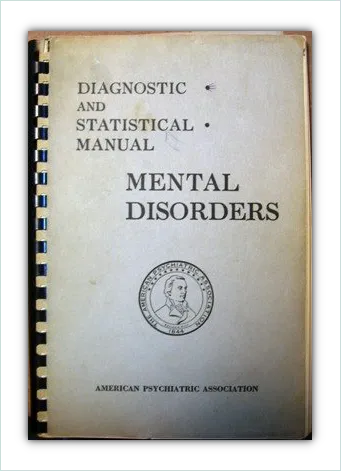
I now know there’s no such thing as a “mental disorder” because I’ve taken the time to research the history of the DSM (the Diagnostic and Statistical Manual of Mental Disorders).
So, to be clear, I now know there’s no such thing as a mental disorder in the way in which we currently think of these.
As in the way the DSM suggests mental health conditions and addictive behaviours to be “disorders”. Or the medical profession suggests them to be mental “illnesses”.
There are no physical markers or symptoms for these conditions, as there are for a proper illness such as a common cold.
The hypotheses and philosophies of psychology are not hard science or medicine.
They’re the opinion of a relatively small demographic of a particular culture. And opinion is regularly skewed by personal perspective, personal bias, personal motivation, politics and, sometimes, financial gain.
At this stage of our understanding, when there’s (once again) a strong and more rational move towards a holistic perspective on mental health, this ongoing creation of disorders is badly informed, ethically questionable and outright irresponsible.
But I only understood more about how a disorder is created when I researched the history of the DSM and how it developed into what is now commonly referred to as the “Bible of psychiatry and psychology”.

I’ve chosen to cite information from credible sources in this chapter because this information is extremely important. Without understanding what a mental diagnosis is, the majority of people who may receive one will probably never be able to get well.
I also know, from past experience, that my authority and knowledge in this arena will be questioned (or ignored) because I’m not a doctor or psychologist.
Everything I’m about to share with you is historical fact, some of it quoted from The American Psychiatric Association’s own website articles and archives.
It shows some interesting connections that only become apparent when the development of the DSM is looked at in chronological order.
Although this proverbial rabbit hole goes even deeper when one begins to examine the background history of some of the individuals involved, and hence understands more about what their underlying personal motivation may have been, the information included should be more than enough to offer people some insight into why they may not be "disordered" at all.
I’ve added explanations below the citations for those who may be put off by the psychological jargon. And, in accordance with standard practice throughout, I’ve made specific bits of information bold for you to take note of.
Like this.
It’s an interesting story and worth reading if you, or those close to you, may prefer a more rational and lasting solution for mental health and addiction challenges.
Professions seem to add enough jargon to confuse laypeople in order to maintain positions of unquestionable authority.
You are intelligent and capable enough to become informed and to make better informed decisions for your health. This professional arena, particularly, has overly complicated things and possibly done this intentionally.
Please take the time to read and consider this chapter thoroughly. I’ve tried to keep it as light and entertaining as possible despite the very serious nature of the content it contains.

The History of the DSM
We tend to think of people like Freud and Jung as the "fathers of psychology". Yet the history of the DSM, which impacts how psychological conditions are viewed and treated on a global scale today, begins in 19th Century America.
And there with the Constitutionally mandated census of 1840.
The 1840 US Census
What might be considered the first official attempt to gather information about mental health in the United States was the recording of the frequency of “idiocy/insanity” in the 1840 (U.S. government) census.1
The Census Bureau added the question at a time when reformers were interested in creating institutions to help people with mental disabilities.2
The 1840 census asked each head of family a variety of questions, but the only ones pertinent to this conversation are:
- The number of free White males and females, respectively: (list of ages)
- The number of slaves and free Colored persons of each sex, respectively: (list of ages)
- The number of White persons who were insane and idiots (at public and private charge)
- The number of Colored persons who were insane and idiots (at public and private charge).3
Insanity or idiocy were decided upon by heads of family and census officials. Not mental health professionals. This resulted in slave owners deciding upon the sanity or idiocy of their slaves, for example.
A mental health diagnosis based on the opinion of a slave owner, skewed by personal perspective, personal bias, personal motivation, politics and, definitely, financial gain.
Slavery was good for Black people, the figures indicated, and freedom led to insanity.4
Specifically, free Black people were far more likely than the enslaved to succumb to insanity. “Insanity and idiocy” was ten times more common among free Black people than among those who were slaves.4
What else could this mean, advocates of slavery asked, but that Black people were mentally unsuited for freedom? 4
The use of diagnosing people as sane or insane for political reasons and financial gain is immediately obvious. As is the danger of the fashionable opinion of society deciding what sane or insane even is.
Regardless of these concerns the government continued to ask these questions in the 1880 U.S. Census.

The 1880 US Census
By the 1880 census, seven categories of mental health were distinguished: mania, melancholia, monomania, paresis, dementia, dipsomania, and epilepsy.5
There are two main categories of mental health conditions at this point:
Psychological reactions: elevated mood, activity and thinking (mania); depression (melancholia); addictive behaviours (monomania); alcoholism (dipsomania).
And physical abnormalities of the brain: epilepsy; dementia; paresis (originally thought to be a result of syphilis, which is physically disease related).
The physical category has structural abnormalities, or disease. The other conditions do not have physical markers of disease or biological abnormalities.
The psychological categories in the 1880 census do not indicate physical markers of illness or disease, because they are not diseases or disorders in the way in which we’ve come to believe they are today.
By this time there was also a growing awareness of cost to State of inpatients in institutions, an ongoing interest in eugenics and some pretty discriminatory personal perspective clouding the air.
Eugenicists theorized that behaviors like criminality and prostitution were products of mental instability, and therefore inheritable traits that “feeble-minded” parents would pass on to their children.2
… nativists feared that these demographic groups were reproducing too quickly for institutions to handle them all.2
... near the turn of the century, scientists and doctors became less interested in helping these people and more interested in preventing them from reproducing. 2
A fear was raised that demographic groups assumed to be more genetically susceptible to “insanity” were reproducing too fast for government institutions to handle them.
Costs to the State became a concern and interest in building institutions to assist people with mental health conditions waned.
There was a consequent shift from helping people with mental health conditions to preventing them from reproducing.
It was around this time, the census stopped asking about mental health.
The AMSAII, however, continued to do this and provided the Census Bureau with their statistics instead.
Who was the AMSAII?
At a meeting in 1844 in Philadelphia, thirteen superintendents and organizers of insane asylums and hospitals formed the Association of Medical Superintendents of American Institutions for the Insane (AMSAII). 6
The group was chartered to focus "primarily on the administration of hospitals and how that affected the care of patients", as opposed to conducting research or promoting the profession.6
The AMSAII were superintendents and organizers of insane asylums with a focus on the administration of hospitals.
In 1893, the organization changed its name to The American Medico-Psychological Association and later, in 1921, became the American Psychiatric Association.

Statistical Manual for the Use of
Institutions for the Insane
In 1917, the American Medico–Psychological Association, together with the National Commission on Mental Hygiene, developed a plan adopted by the Bureau of the Census for gathering uniform health statistics across mental hospitals. 1
Although this system devoted more attention to clinical usefulness than did previous systems, it was still primarily an administrative classification.1
It was specifically designed for administrators of inpatient mental hospitals to use for collecting institutional data, rather than for guiding treatment of specific patients. [my boldface] 1
This Statistical Manual for the Use of Institutions for the Insane (often confused with the subsequent DSM) was never intended to be used for diagnosing people and the word “diagnosis” is not even mentioned in the title.
It was a manual, created for administrative purposes only, to share statistics between institutions and the government.
The Census Bureau was still gathering information on mental health, but now from institutions via this administrative manual.

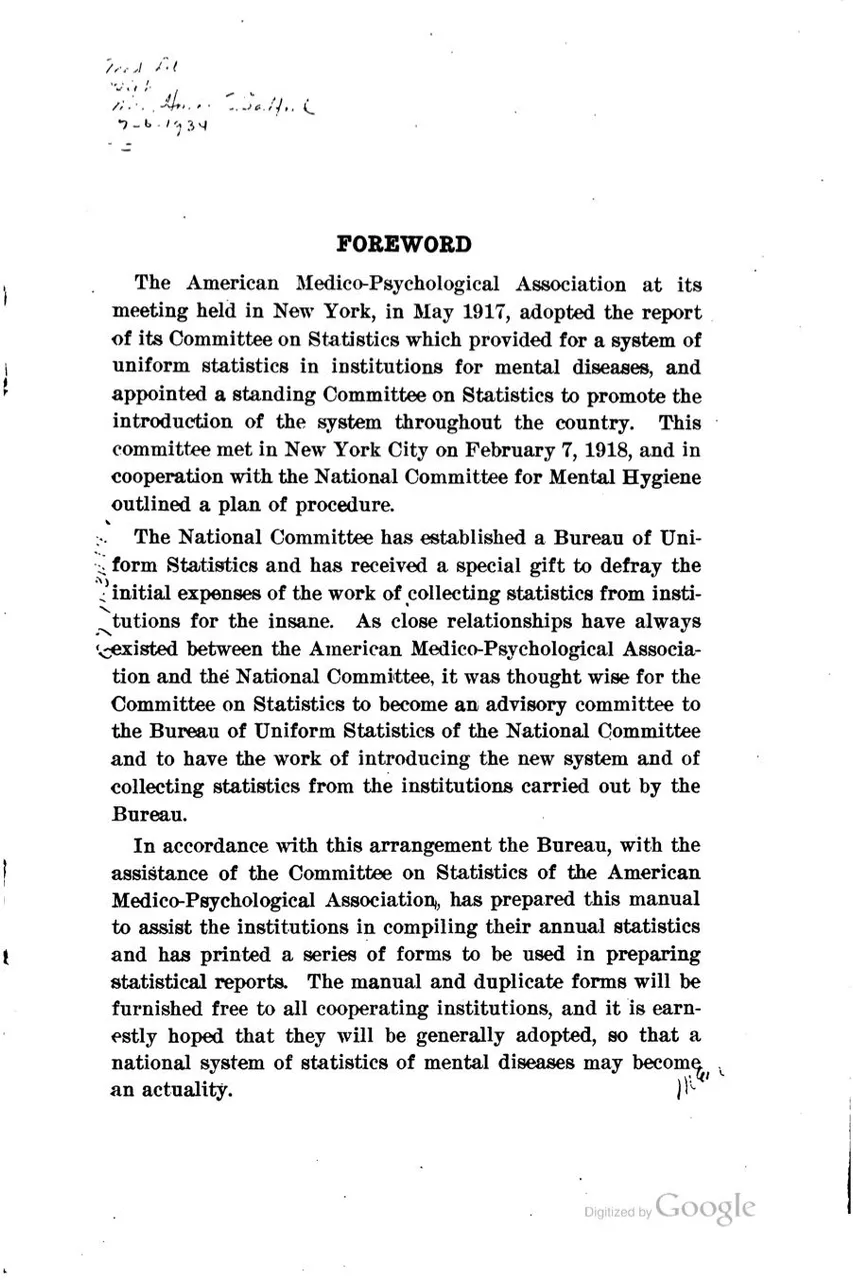

In the Statistical Manual for Use of Institutions for the Insane:
Of its 22 principal groups only one, the psychoneuroses, reflected conditions found in noninstitutionalized patients.7
In other words, the only group of conditions found in non-institutionalized patients (as well as those in institutions) are the “neuroses”. These “neuroses” were characterized by an anxiety that seemed disproportionate to the present situation.
The statistical manual (for Use of Institutions for the Insane) also reflected the view that the conditions it classified arose from somatic (relating to the body as opposed to the mind), constitutional (relating to someone’s general state of health), and heredity (genetic) factors.7
Here we have what is now called Biological psychiatry.
The perspective that mental health conditions arise due to physical abnormalities/biological factors. Accordingly, treatments for such were somatic therapies i.e. physical intervention to the brain, body and nervous system functions.
Lobotomy anyone?

Treatments Change With Knowledge
Doctor Knows Best
Lobotomy, also called prefrontal leukotomy, surgical procedure in which the nerve pathways in a lobe or lobes of the brain are severed from those in other areas. The procedure was formerly used as a radical therapeutic measure to help grossly disturbed patients with schizophrenia, manic depression and mania (bipolar disorder), and other mental illnesses.8
Evidence that surgical manipulation of the brain could calm patients first emerged in the late 1880s, when Swiss physician Gottlieb Burkhardt, who supervised an insane asylum... performed his operation on six patients, with the specific purpose not of returning the patients to a state of sanity but of putting them into a state of calm [my boldface]. 8
One of Burkhardt’s patients died several days following the operation, and another later committed suicide. 8
Regardless, the lobotomy took off as a medical procedure to treat mental health.
Lobotomies were performed on a wide scale during the 1940s; ... The practice gradually fell out of favour beginning in the mid-1950s, when antipsychotics, antidepressants, and other medications that were much more effective in treating and alleviating the distress of mentally disturbed patients came into use.[my boldface] 8
Chemical lobotomy anyone?
But how did the switch to a chemical intervention of brain function become popular and was the perspective of Biological psychiatry good medicine?
Please read on.

Post World War II
By this time, most mental-health professionals practiced in community sites, not in mental hospitals. 7
The Statistical Manual (for Use of Institutions for the Insane) offered little guidance for clinicians in outpatient settings. The psychotic conditions that dominated its classifications were no longer of high priority for the majority of therapists. 7
In addition, clinicians who used psychodynamic perspectives that stressed psychological and social processes were coming to dominate outpatient psychiatry [my boldface]. They had little use for the biological explanations that the Statistical manual (for Use of Institutions for the Insane) reflected.7
Mental health professionals at this point (after WW II) were largely working with people who were not hospitalized. These professionals were less interested in blaming genetics or physical abnormalities of the brain and more interested in a psychoanalytical approach to uncover the reasons why a person may have been suffering.
These mental health professionals were aware the war veterans they were trying to treat had a logical reason to be mentally distressed.
A much broader classification system was later developed by the U.S. Army (and modified by the Veterans Administration) to better incorporate the outpatient presentations of World War II servicemen and veterans (e.g., psychophysiological, personality, and acute disorders).7
The U.S Army then developed its own mental health classification system based on what reactions and mental health challenges were being exhibited by its war veterans.
At the same time, the World Health Organization (WHO) published the sixth edition of the ICD (ICD-6), which, for the first time, included a section for mental disorders.7
ICD is the acronym for “International Classification of Diseases”.
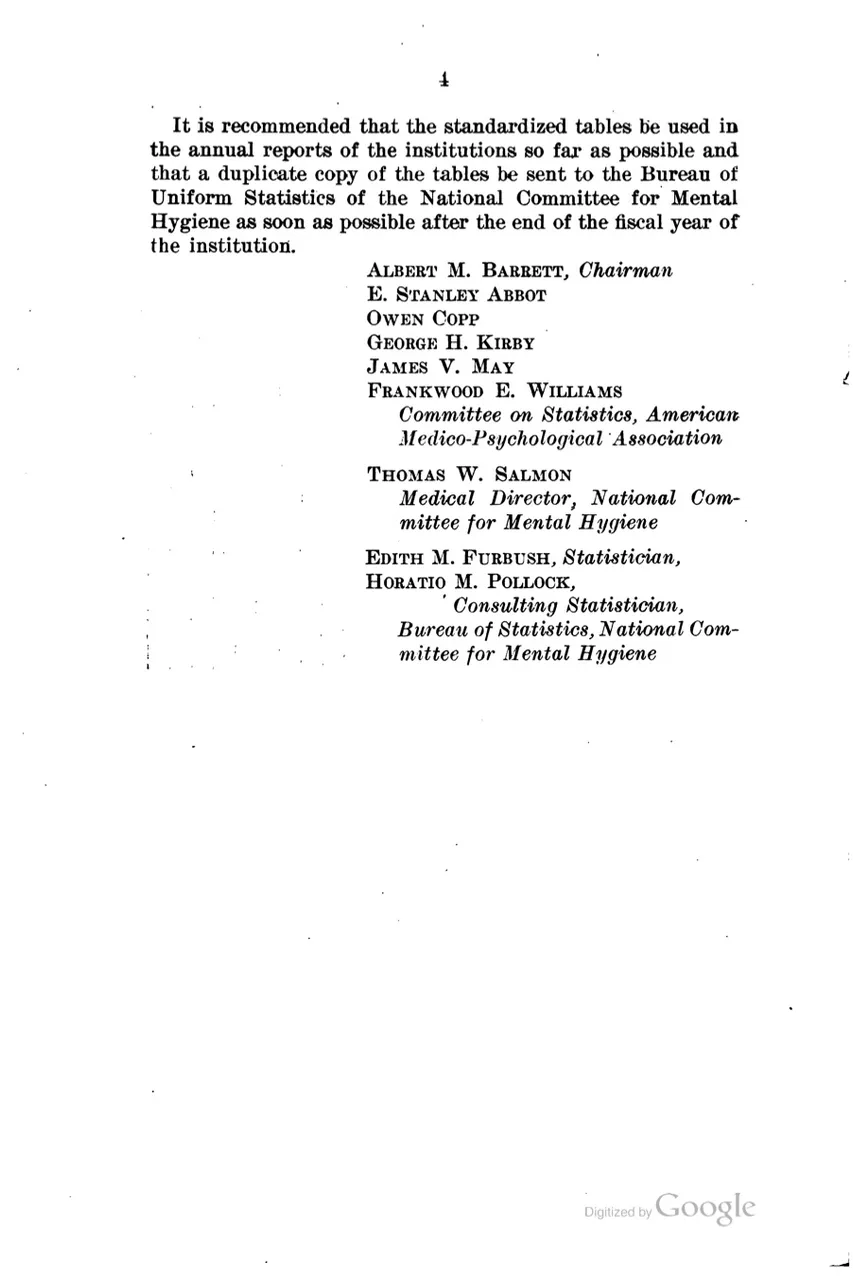
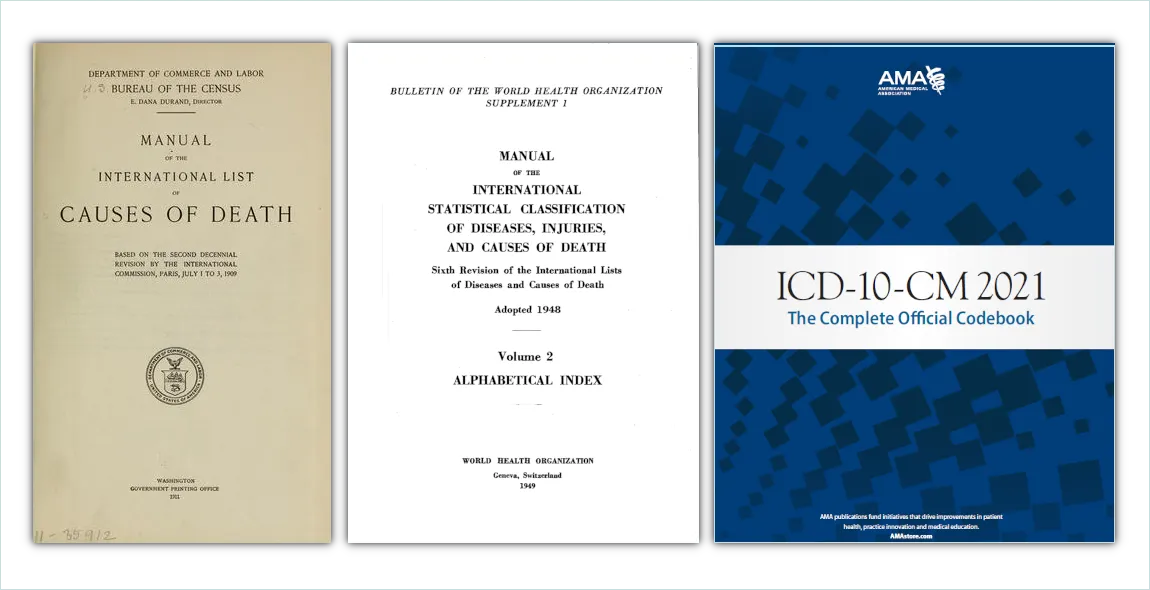
Today there are two established systems for classifying mental disorders:
- The DSM (Diagnostic and Statistical Manual of Mental Disorders)
- The ICD (International Classification of Diseases)
It is commonly thought that Europe generally uses the ICD to diagnose mental health disorders, while The U.S.A and a variety of other countries uses the DSM as their diagnostic tool.
But, in fact, both are referred to for treatment and the two have been inextricably linked from their early development, which would explain why:
ICD–6 was heavily influenced by the Veterans Administration classification [my boldface] and included 10 categories for psychoses and psychoneuroses and seven categories for disorders of character, behavior, and intelligence. 1
So let's have a quick look at the development of the ICD, how this is connected to the DSM and what the implications of this may be.

International Classification of Diseases (ICD)
International Classification of Diseases [my boldface] (ICD), in medicine, diagnostic tool [my boldface] that is used to classify and monitor causes of injury and death and that maintains information for health analyses, such as the study of mortality (death) and morbidity (illness) trends. 9
The ICD is designed to promote international compatibility in health data collecting and reporting [my boldface]. 9
The ICD also lists diseases and assigns codes to them. These codes are used for medical administration purposes and medical insurance claims.


The History of the ICD
Some scholars track the origin of ICD to 1763. The French physician and botanist Dr François Bossier de Sauvages de Lacroix developed a categorization of 10 distinct classes of diseases, which were further divided into 2400 unique diseases.10
Fully classifying a medical condition requires knowing its cause (and that there is only one cause), the effects it has on the body, the symptoms that are produced, and other factors [my boldface]. 11
For example, influenza is classified as an infectious disease because it is caused by a virus, and it is classified as a respiratory infection because the virus infects and damages certain tissues in the respiratory tract. 11
The more that is known about the disease, the more ways the disease can be classified nosologically. 11
Nosology (from Ancient Greek νόσος (nosos) 'disease', and -λογία (-logia) 'study of') is the branch of medical science that deals with the classification of diseases. Definitions from Oxford Languages
François Boissier de Sauvages de Lacroix's classifaction was based on actual physical diseases and viruses.
But then he wrote a treatise...
Sauvages de Lacroix explained his nosology in the 1763 treatise Nosologia Methodica, a work that reportedly was an inspiration to Philippe Pinel (1745—1826) and his early research of mental illnesses. 12
And Philippe Pinel...
... made notable contributions to the classification of mental disorders and has been described by some as "the father of modern psychiatry". 13
It would make sense, then, that the "biological" approach to psychiatry became so easily accepted right from the beginning.
At least, this set up mental reactions to be easily confused with the classification and nomenclature of proper diseases. Or, at the very least, to be heavily influenced by this.
Isn't it interesting how personal interests and personal perspective influence "science"?

And then the interest grew...
Recognizing the importance of disease classification, the first International Statistical Congress held in Brussels in 1853 appointed Jacob Marc d'Espine and William Farr to develop a system of classifying causes of mortality that could be used across borders and languages. 14 original citation removed from WHO website
This was the genesis of what became known as the “International List of Causes of Death.” (ILCD) 14
Two statisticians were initially recruited, by the Congress, to come up with an internationally uniform system of classification for diseases and mortality rates.
William Farr and Jacob Marc d'Espine.
William Farr had been encouraging administrative bodies to institute a formal disease classification since he'd been approached by Florence Nightingale upon her return, to England, from the Crimean War.
After she had returned to England, Florence Nightingale:
...promoted the importance of and the need for hospital data and statistics on causes of illness and causes of death in the armed forces at the political level, and she enlisted the aid of Farr to work on the technical aspects of these problems. 15
Farr had already been employed at the General Register Office of England and Wales since 1939.
... and he, probably more than anyone else, developed and analyzed mortality statistics to delineate the sanitary and health problems of the day. 15
In the first Annual Report of the Registrar General (12), therefore, he (Farr)... urged the adoption of a uniform classification as follows:
"The advantages of a uniform statistical nomenclature, however imperfect, are so obvious, that it is surprising no attention has been paid to its enforcement in Bills of Mortality. Each disease has, in many instances, been denoted by three or four terms, and each term has been applied to as many different diseases: vague, inconvenient names have been employed, or complications have been registered instead of primary diseases. The nomenclature is of as much importance in this department of inquiry as weights and measures in the physical sciences, and should be settled without delay." 16
William Farr and Jacob Marc d'Espine created their own nosological classifications independently. Although they respected each other's work, they were at odds on the nomenclature chosen for their respective systems of classification.
After summarizing Farr's results, he (Marc d'Espine) gave details of the nosological classification used, and criticized its main division of diseases into "epidemic" and "sporadic", preferring instead that of "acute" and "chronic". 17
Farr replied promptly in a long footnote in the next Annual report of the Registrar-General. 4 He described Marc d'Espine's work approvingly, but rebutted his criticisms of the nosology. 17
Clearly, the importance of words was noted right from the beginning of these attempts at classification.
Due to Farr and d'Espine being unable to resolve the differences between their preferred terms/names, both forms were offered for consideration at the Paris Congress in 1855.
Farr and d'Espine submitted two separate lists of the causes of death.
Farr’s system was arranged under 5 groups of diseases: epidemic diseases, constitutional [my boldface] (general) diseases, local diseases arranged according to anatomical site, developmental diseases, and diseases as the direct result of violence. 18
D'Espine classified diseases according to their nature (gouty, herpetic, haematic, etc.). As a compromise between the views of Farr and d'Espine, the congress adopted a compromise list of 139 groups of diseases. 18

William Farr
By Unknown author - Popular Science Monthly Volume 23, Public Domain
Original Image Source

Marc d'Espine
Porträt, um 1858. Nach einer alten Fotografie (Bibliothèque de Genève) found on HLS website

The Congress compromised and combined the lists but, after reading more on this, it seems Farr's list may have had a bit more influence on the final outcome.
Of the classification approved by the Congress:
.. The list was "classified" in the sense that it grouped causes of death roughly, but not in accordance with either of the two proposals: its two main classes were "well-defined diseases" and "incompletely-defined diseases". Congress left the choice of classification system unresolved. 17
It must be admitted that at both Paris and Vienna there was considerable opposition to the desirability, or even possibility, of a standard list of causes of death. 17
Some doctors present argued that statisticians had no right to dictate to medical men; that even a purely medical congress would find it impossible to agree on such a list; and that it would be an obstacle to progress and an infringement of their freedom to name diseases as they chose [my boldface]. Again Congress reached no conclusion. 17
Marc d'Espine, however, was concerned about the decisions made.
After the Vienna Session... Marc d'Espine wrote an entire book to support his case... he pressed the need for 'me'decins verifcateurs'to check the causes of death entered by general practitioners [my boldface]. 17
In the event, this did not matter, as Marc d'Espine had died on 15 March 1860, four months before the session opened. The International Statistical Congress held another five full sessions before its sudden collapse in 1878, but the subject of a standard international nosology was never raised again 17
The work of William Farr and Jacob Marc d'Espine would lay the foundation of what was to become the “International List of Causes of Death”

Marc d'Espine's work was restricted to the small canton of Geneva, but it was not unknown elsewhere, nor did he labour in isolation. There survive seventeen letters he wrote... to Adolphe Quetelet, the famous Belgian astronomer and founder of the International Statistical Congress. 17
The International Statistical Institute adopted the first international classification of diseases in 1893. The system was based on the Bertillon Classification of Causes of Death, developed by French statistician and demographer Jacques Bertillon. 19

Adolphe-Louis Jacques Bertillon
Bibliothèque nationale de France, Public domain, via Wikimedia Commons

Jacques Bertillon... was a French statistician and demographer whose application of quantitative methods to the analysis of a variety of social questions gave impetus to the increased use of statistics in the social sciences. 20
Bertillon worked to establish uniform international statistical standards and saw his “Bertillon classification” of causes of deaths come into use in many nations. 20
Educated as a physician, but with a later focus on statisicts, one of Bertillon's main areas of interest was the rise of alcoholism in France. He wrote a paper on the subject titled "L’Alcoolisme et les moyens de le combattre jugés par l’expérience". (1904; “Alcoholism and Ways of Combating It Judged from Experience”)
This may explain how the "disease model" (the idea that alcoholism is a disease) became widely accepted as "medicine".
At around that time, the “(Bertillon) [added by me] International List of Causes of Death was presented in the United States at the International Statistical Institute, and in 1898, various countries in North America, including the United States, adopted this system. 14
When the U.S.A adopted the system, it did so under the proviso that the classification list was to be revised roughly every ten years.
This was agreed upon and the next revisions took place in 1909, 1920, 1929 and 1938.

The Fifth Revision Conference
The Fifth International Conference for the Revision of the International List of Causes of Death [my boldface] (ILCD)... was convened by the Government of France and was held in Paris in October 1938. 16
... the Conference recognized the growing need for a corresponding list of diseases to meet the statistical requirements of widely differing organizations, such as health insurance organizations, hospitals, military medical services, health administrations [my boldface], and similar bodies. 16
At this point, it was suggested that the classification lists of both diseases and deaths were combined into one manual.
The Conference also recommended that the United States Government continue its studies of the statistical treatment of joint causes of death "warmly" thanking the U.S.A, in it's resolution, "for the work it has accomplished or promoted in this connection".
And ordered that:
Pending the compilation of international lists of diseases, the Conference recommends that the various national lists in use [my boldface] should, as far as possible, be brought into line with the detailed International List of Causes of Death. [my boldface] 16

Sixth Revision of the International Lists
The International Health Conference held in New York City [my boldface] in June and July 1946 entrusted the Interim Commission of the World Health Organization with the responsibility of: 16
reviewing the existing machinery and of undertaking such preparatory work as may be necessary in connection with: 16
(i) the next decennial revision of 'The International Lists of Causes of Death' (including the lists adopted under the International Agreement of 1934, relating to Statistics of Causes of Death); and
(ii) the establishment of International Lists of Causes of Morbidity 16
To meet this responsibility, the Interim Commission appointed the Expert Committee [my boldface] for the Preparation of the Sixth Decennial Revision of the International Lists of Diseases and Causes of Death. 16This Committee, taking full account of prevailing opinion concerning morbidity and mortality classification, reviewed and revised the above-mentioned proposed classification which had been prepared by the United States Committee [my boldface] on Joint Causes of Death. 16
The Committee also compiled a list of diagnostic terms [my boldface] to appear under each title of the classification. 16

The International Conference for the Sixth Revision... was convened in Paris from 26 to 30 April 1948 by the Government of France under the terms of the agreement signed at the close of the Fifth Revision Conference in 1938. 16
Its secretariat was entrusted jointly to the competent French authorities and to the World Health Organization [my boldface], which had carried out the preparatory work under the terms of the arrangement concluded by the governments represented at the International Health Conference in 1946. [Off.Rec. Wld. Hlth Org., 1948, 11, 23.] 16
The Conference adopted the classification prepared by the Expert Committee [my boldface] as the Sixth Revision of the International Lists. 20 [Off.Rec. Wld. Hlth Org., 1948, 2, 110] 16
Here we see why the sixth revision of the ICD (ICD-6),
... which was adopted from the classification prepared by the "Expert Committee",
... who was put in place by the "Interim Committee" of the "WHO" (that didn't exist yet),
... but who "reviewed and revised the above-mentioned proposed classification prepared by the United States Committee",
... may be said to be "heavily influenced by the U.S. war veterans manual'.
And, perhaps, a bit more.
Because it's at this point that a list of diagnostic terms were added to each title of the classification.

But who is WHO?
The World Health Organisation (WHO) was founded on 7 April 1948.

By Font: Adrian FrutigerLogotype: The World Health Organization - Website and publications of the World Health Organization:Source 1Source 2, Public Domain
Their founding year, 1948, was the same year they took charge of the decennial revision of the list (ILCD).
On 7 April 1948, only a fortnight prior to the The International Conference for the Sixth Revision of the International Lists of Diseases and Causes of Death, WHO suddenly appears.
I'm uncertain as to how there could have been an "interim commission" for an organization that was not yet in place, or why The International Health Conference held in New York City would entrust them with the responsibilities mentioned above.
Or why this "Interim Commission" for WHO would appoint an "Expert Committee" to review and revise a proposed classification system prepared by the United States Committee.
Or why the The International Conference for the Sixth Revision of the International Lists of Diseases and Causes of Death "adopted the classification prepared by the Expert Committee as the Sixth Revision of the International Lists." [Off.Rec. Wld. Hlth Org., 1948, 2, 110] 16
But it was at this point that diagnostic codes were added to the list/manual as well:
In 1948, the World Health Organization (WHO) took charge of the classification system, which was expanded the following year to include coding for causes of morbidity [my boldface] in addition to mortality. 14
I do know that hospitals and medical professionals use these same codes, from the ICD, on their client invoices. And that these codes are required by medical insurance companies for medical cover and reimbursement.
In addition:
The system was rechristened the International Classification of Disease system. (ICD) [my boldface] 14


Surprisingly similar development to the DSM, isn't it?
Both manuals initially being developed for statistical reasons.
Both manuals transforming into medical diagnostic tools for mental "disorders", for which there are no physical markers of disease.
Both manuals keeping almost identical acronyms, even though the title of the manuals were completely changed.
International List of Causes of Death (I L CD) to: Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Death.
Or, these days, just International Statistics Classification of Diseases. (ICD)
Diagnostic Statistical Manual for Institutions for the Insane to: Diagnostic Statistical Manual of Mental Disorders (DSM commonly used to refer to both).
And although the current ICD is generally seen as independent to the DSM, there is a clear connection between the manuals and a European and American collaboration during their development.
And now we return to Post War America.

Post World War II (cont)
A recap:
The Statistical Manual (for Use of Institutions for the Insane) was not helpful to clinicians working in outpatient settings. Clinicians in these settings were also well aware that the patients they were attending to had good reason for their challenges in a post war situation.
These clinicians are were subsequently more interested in a "psychodynamic" approach to treating their patients.
A wider classification system, that incorporated the outpatient mental health challenges of its veterans, was also developed by the U.S Military and modified by its Veterans Administration around this time.
At the same time, the World Health Organization (WHO) published the sixth edition of ICD (ICD-6), which, for the first time, included a section for mental disorders [my boldface]. 20

So, heavily influenced by information gathered by the U.S.A military on the mental health challenges of its war veterans, WHO added the U.S Army’s data to their international classification of diseases.
Despite there being no physical markers or physical symptoms of any kind of disease or illness.
WHO did, however, acknowledge there were mental health categories that were disorders of character, behaviour and intelligence (and not of the brain itself) in their classification of diseases manual.
And now we have a better understanding of why and how the ICD-6 was "heavily" influenced by the American War Veterans system of Classification.
Let's continue looking at how the American Diagnostic Statistisical Manual for the Use of Institutions for the Insane, became the DSM of today.

A war Veteran would, in all likelihood, return from an ongoing high conflict situation with trauma in the form of Post Traumatic Stress Disorder (PTSD) and Complex Post Traumatic Stress Disorder (C-PTSD, which was only first acknowledged in 1992).
At this point there was little understanding of what PTSD and C-PTSD were, or what perceptions, feelings and behaviours are displayed by a person with PTSD and C-PTSD.
So the U.S army creates a mental health classification system based on their war veterans (who would all be suffering from PTSD/C-PTSD) and the ICD uses this to create their world wide categories of mental illnesses/disorders.
And following this…
The APA (American Psychiatric Association) Committee on Nomenclature and Statistics developed a variant of the ICD–6 that was published in 1952 as the first edition of DSM (DSM-I).
20

Original Image Source

The administrative Statistical Manual for Use of Institutions for the Insane is then replaced with the first edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-I).
It was at this point the word “Diagnostic” was added and the words “of Mental Disorders” replaced the words “for the Use of Institutions for the Insane” in the title of the manual.
It was at this point the Statistical Manual (for Use of Institutions for the Insane) transformed into the primary reference book that the majority of mental health professionals use to diagnose mental health disorders in both clinical and community settings in the U.S.A.
And a great many other countries as well.
It was at this point it became the “Bible of psychiatry and psychology” as we know it today.
Developed off the back of a hospital administrative manual that was never meant to be a guide to treating people. Which was aimed at classifying inpatients who were severely impaired enough to be institutionalized.
With a biological perspective on the causes of mental health conditions that encouraged pretty barbaric and dangerously radical physical interventions as treatments. Off the back of a government census that relied on census officials, heads of families and slave owners to decide who was or was not sane.
As a variant of WHO’s manual of International Disease Classifications, which was heavily influenced by mental health classifications by the U.S military service of its war veterans.
Who were probably struggling with as yet undiagnosed, misdiagnosed and misunderstood PTSD and C-PTSD.
What could possibly go wrong?

The Lithium Experiment
Interestingly enough, the use of lithium to treat mental health conditions was first tested by John Cade in Australia in 1948.
Cade had tested the use of Lithium on himself and had experienced no adverse effects. He then decided to try it on Bill Brand, a patient who had been psychotic and institutionalised for around thirty years.
Within a few weeks Bill Brand's condition had substantially improved.
Within about two months, of beginning treatment, he was able to return home.
Brand then stopped taking the medication and his mental health declined, to the point that he was returned to the institution, again. Without knowing the correct dosage due to it being an experimental treatment, Cade upped the dose and Bill Brand died.
Cade began his experimental use of Lithium on Bill Brand in March 1948.
One month prior to the Sixth Revision of the International Lists, the sudden appearance of the World Health Organisation and the addition of a new section of mental disorders, diagnostic terms and a coding system to the ICD.
A few years later, in the same year that the first U.S. Diagnostic Manual (DSM-I) was published (1952), what was soon to become the psychiatric drug of choice at the time, Chlorpromazine, was given to a patient.
In the same decade, Julius Axelrod carried out research into the brain’s neurotransmitters that won him the Nobel Prize for Physiology and Medicine.
This was impetus for further development of psychiatric medicines as neurochemistry became better understood.
And so began the rise of psychiatric medication.
Lithium is still listed on the World Health Organizations List of Essential Medicines in the 22nd List - 2021.

How Things Change
The DSM-I
We now know the DSM-I was developed due to the change of circumstances in treating people with mental health conditions after the war:
The critical impetus for developing a new manual that would reflect the realities of mental health practitioners in the postwar era stemmed from the experiences of military psychiatrists during World War II. This group, led by William C. Menninger, found that the Statistical manual (for the Use of Institutions for the Insane) was a poor fit with the psychiatric casualties of the war. 7
About 90% of these involved men (who) had experienced brief, but intense, reactions to extremely stressful conditions. Only a small minority, therefore, matched the types of cases typically found in mental hospitals. 7
In addition, psychiatrists' wartime experiences taught them that mental disorders often arose because of psychosocial factors [my boldface] rather than the somatic processes that the existing classifications emphasized. 7
The Statistical manual (for the Use of Institutions for the Insane) was becoming obsolete due to the shifting nature of understanding about mental illness coupled with the new types of psychosocial problems that patients were bringing to outpatient settings. 7
A profession that used psychodynamic concepts to understand patients and psychoanalytic techniques to treat them required a nomenclature applicable to its new outpatient clientele. [my boldface] 7
Mental health practitioners suddenly found the Diagnostic Statistical Manual for the Use of Institutions for the Insane unhelpful for the war veterans they were trying to assist, because only a small minority of the war veterans (in outpatient settings) matched the cases in mental hospitals.
Mental health practitioners, now working with outpatients, were also aware that the war veterans they were trying to treat had been exposed to extremely stressful situations.
Mental health practitioners trying to assist these war veterans had a more rational, psychosocial perspective on mental health challenges.
psychosocial
adj. describing the intersection and interaction of social, cultural, and environmental influences on the mind and behavior. 22
The relationship between psychological factors and the physical body can be influenced by social factors, the effects of which are mediated through psychological understanding. 23
Examples of psychosocial factors include social support, loneliness, marriage status, social disruption, bereavement, work environment, social status, and social integration. 23
Many mental Health professionals believed social factors like loneliness, bereavement etc., as well as the environment influenced psychological and physical states.
Outpatient clinicians found the need for different terminology to be agreed upon in order to be able to address this new post war situation and, in response, the American Psychiatric Association created a new manual to classify mental health conditions.
In the first edition of the Diagnostic and Statistical Manual for Mental Disorders (DSM-I), there was a more psychodynamic perspective as opposed to the purely biological approach (purely physical/genetic reasons for mental health challenges) of mental hospitals.
“Psychodynamics” looks at how a person's psychology (perception and thinking) impacts their behaviour, feelings and emotions, in relation to external factors and early experience.
… it (the DSM-I) combined the psychoanalytic approach of Sigmund Freud, which emphasized the unconscious forces that he presumed to underlie mental illness, with the life-course approach of American psychiatrist Adolf Meyer, which focused on how mental illnesses were reactions to challenges that individuals faced in adjusting to their environments [my boldface].
It made no sharp distinctions between mental illness and mental health [my boldface]. 7
It was driven by psychodynamic assumptions that were more concerned with the underlying problems patients had than with the overt symptoms they displayed. 7
In other words, clinicians were focused on treating the reasons that people were suffering instead of medicating the overt symptoms they displayed.

In the DSM-I, mental health conditions were still separated into two major groups.
Physical/biological abnormalities
Psychological reactions.
But there was a new trend towards understanding how past experience, external environment and current perception impact brain and physical function, instead of the prior belief that biology was entirely responsible for mental health conditions.
The DSM-I listed category names, with a brief paragraph describing the behaviours associated with them.
The category names used the word “reactions” to explain the behaviors associated with them, instead of the word “disorders” we see added to every category name today.
This is a far more accurate observation of mental health challenges and might be far more beneficial, for successful treatment, for those who are suffering with them.

The DSM-I:
called all the functional disorders “reactions” [my boldface] (e.g., “schizophrenic reaction” or “depressive reaction”) because, unlike organic brain disturbances, they arose in response to patients' life histories and social environments [my boldface]. 7
At the heart of DSM-I and DSM-II was the concept of “neurosis.” It was the synthesizing rationale behind the manual's psychoneurotic category, which was the category at the center of clinical practice. 7
In other words, many mental health practitioners believed the underlying cause of all mental distress (that was not due to physical trauma/abnormality of physical brain structure) was caused by neurosis.

neurosis
noun [ C or U ]
a mental illness resulting in high levels of anxiety, unreasonable fears and behaviour and, often, a need to repeat actions for no reason. 24
According to Sigmund Freud (1856-1939), a famous Austrian neurologist who founded the discipline of psychoanalysis, neurosis is a coping strategy caused by unsuccessfully repressed emotions from past experiences. 25
He gave the example of an overwhelming fear of dogs that may have resulted from a dog-attack earlier in life. 25
A conflict between two psychic events: Carl Gustav Jung (1875-1961) was a Swiss psychiatrist who founded analytical psychology. He believed that a neurosis was a clash of conscious and unconscious events in the mind. 25
These stances on neurosis confirm that it is seen as an ailment, and is normally discussed with an aim to finding the cause of and treating the condition [my boldface]. While a personality test can confirm that a person has neuroticism, it is not a disease or condition and cannot be “treated.” [my boldface] 25

With a focus on psychoanalytic theory, mental health practitioners viewed the categories of behaviours (now called mental disorders) as neuroses that were created by an underlying conscious or unconscious anxiety.
The subsequent behaviours associated with these neuroses were adopted as an attempt by the individual to manage this anxiety.

The description in the DSM-I for the main Psychoneurotic reactions category read:
"The chief characteristic of these disorders is “anxiety” which may be directly felt and expressed or which may be unconsciously and automatically controlled by the utilization of various psychological defense mechanisms (depression, conversion, displacement, etc.) 26
…“Anxiety” in psychoneurotic disorders is a danger signal felt and perceived by the conscious portion of the personality [my boldface].
It is produced by a threat from within the personality (e.g., by supercharged repressed emotions [my boldface], including such aggressive impulses as hostility and resentment), with or without stimulation from such external situations as loss of love, loss of prestige, or threat of injury.” 26

This definition indicates the extent to which psychodynamic assumptions infused the DSM-I classifications. [my boldface] 7
Anxiety, by definition, expressed defense mechanisms that were largely unconscious and that emerged from some inner threat [[my boldface]. 7
Moreover, the ways patients expressed anxiety, through such mechanisms as “depression, conversion, or displacement [my boldface],” were secondary [my boldface] to the fundamental process of anxiety that was behind each overt manifestation. 7
The "disorders" of today (e.g BiPolar Disorder) were only considered to be the symptoms/reactions to this main underlying cause of conscious or unconscious anxiety by many clinicians in the 1950’s.
Depression was considered to be a reaction to an underlying anxiety, such as a repressed threat of assault which may have been experienced in the past, that was triggered as a coping mechanism when a person was reminded of the past event.
The Bipolar reactions (mania, depression) were not disorders in and of themselves.
Which is what we have been led to believe they are today (“BiPolar Disorder”).
Or worse... that the person themselves is disorderd. (He/She is BiPolar)
Manic and depressive sypmtoms were considered to be reactions, set off by environmental circumstances that had triggered conscious or unconscious memories of unresolved trauma.

So in accordance with this more rational, logical and psychodynamic approach to mental health challenges the DSM-I refers to depression as “Depressive Reaction” and has the following description:
“The anxiety in this reaction is allayed, and hence partially relieved, by depression and self-depreciation. The reaction is precipitated by a current situation, frequently by some loss sustained by the patient, and is often associated with a feeling of guilt for past failures of deeds.” 26 (American Psychiatric Association, 1952, pp. 33–34)
In other words, something in a current situation brings this anxiety into play and the reaction (depressive reaction for example) relieves the anxiety in some way.
The description of depressive reaction also mentions that the reaction “is often associated with a feeling of guilt for past failures of deeds”.
Guilt and shame are primary feelings associated with unresolved trauma.
And “anxiety” (or the constant sensation of being on “high alert”) is one of the most common effects of unresolved Post Traumatic Stress Disorder Reaction.
From here on I’m reverting to the psychodynamic perspective when discussing mental health conditions. As used by the DSM-I, I’m replacing the word “disorder” with “reaction”.
I’m also replacing the word “symptoms” and any other medicalised reference to these reactions with a term that is more in line with a psychoanalytic perspective.
Because these are not “medical illnesses”.
And these are not incurable "disorders" in my personal experience.
My reasoning will make sense if you read on.

Citations, Bibliography and additional source material >

I do not endorse the information shared in K.I.S.S - Keep it Simple Sweetheart Perfect to be used in place of professional medical advice, support groups or specific therapies.
Please do not come off any prescribed medication without the guidance and support of a trained professional.
Please do not step away from any programs of treatment or support groups without the guidance and support of a trained professional.
