A hematoma is a collection of blood anywhere in the body. It looks more of a bruise with a lump under it, where it can be hard or soft, that can just be dispersed slowly when pressed or left alone. Where most people will just apply a cold or hot compress over it and the problem is solved.
In the medical field, the issue is on where hematomas are developed.
Anyone who have had peripheral venflons when they're in the hospital know that these access the veins for reasons of having medications, intravenous fluids or just an instant access when needed. As the vein is punctured, necessary observations are needed ie. bleeding inside or outside the puncture site. This among other reasons that can happen with it.
In Cardiology, we need bigger veins and in Cath Lab, we also need an arterial access, the bigger ones are in the groins...the femoral veins and arteries.
For years now, angiograms, with or minus angioplasty, is possible using the Right radial artery in the wrist, or the Left if the other is not possible. After the procedure, it is easier for the patients as they don't need to lie flat for an hour or more, with less or no limitations. They can eat, drink and get out of the bed for toilet needs.
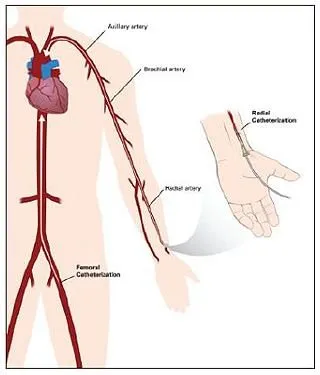
Disclaimer: image from premierhealthspecialists.org
As the radial arteries are narrower, the need to use the femoral arteries in the groin is a possibility for each patient. Other procedures warrant it as the only access.
All in a day's work
Yesterday shift was a typical day, our Coronary Care Unit (CCU) receiving patients from the cath lab, one elderly in particular had her aortic valve done, accessed trans-femorally. With a massive hematoma but already attended to from the cath lab.
When she came to the ward, the surrounding areas of the puncture site were lumpy, the puncture site was not soft, alerting my colleague to call the doctors who did the procedure. The blood pressure then dropped to half of the patients's BP. On examination of the hematoma, it have grown harder and a bit bigger.
The patient was bleeding.
Managing a femoral hematoma
Actually, a femoral artery is not that deep. Plus the arterial pulsation shows where the pulse is. But because it is beside the vein, it is important to access it as the procedure warrants its' use. Both the vein and the artery have specific uses, it can't be interchanged.
Bleeding and hematomas can occur anytime during the procedure with immediate management. Bleeding can also occur anywhere in the artery, not just from the puncture site. I will focus on bleeding and hematomas from the puncture site for now.
Either simple or complicated procedure, radial or femoral, after care is the same, IDEALLY. Protocol says that the site needs to be assessed every 30 minutes for 2 hours, the length of time depends on how much Heparin was given to the patient.
With the femoral access, the patient needs to lie flat, with the affected leg straight.
Here is the reason WHY. Sometimes, there is an absorbable PLUG that is applied to the punctured artery to stop it bleeding. It is sensitive in its application, it can be dislodged. Or even if there's no plug, closing the access manually is being done too. Movements like turning to sides, flexing the leg can produce bleeding, inside or outside the skin. Unnoticed, unchecked, mismanaged appropriately, BLEEDING CAN HAPPEN. Under the skin, HEMATOMA can developed.
Believe it or not, there shouldn't be any problem when attended to and managed immediately. We have managed a lot of hematomas in our lifetime, but the one thing that a manual compression can't managed is this: AN ONGOING BLEED UNDER A HEMATOMA.
Or a trickly ooze or bleed.
Imagine a massive hematoma over an arterial bleeding puncture. No matter how deep is the compression, reaching the artery is impossible. The bleeding can only be stopped surgically so our patient went back to the cath lab for surgical repair.
Any further complications?
Our patient's BP dropped, giving her liters of IV fluids. Her hemoglobin also dropped, giving her a few units of blood. These are just immediate complications that can be managed easily.
A much worse complication can still happen from here. A debilitating complication that can easily happen from a hematoma. A friend in cath lab reported of removing a lot of clots afterwards. Also, after the repair, the flow of blood in the leg was sluggish.
Years ago, a patient's lower leg was surgically amputated after having a hematoma. During that time that the bleeding was ongoing, those blood were intended to flow to the lower leg.
A heart muscle cell, an arm or a leg with insufficient blood supply will die. Whereas dead heart muscle cells can affect the pumping action of the heart, a limb needs to be amputated before it can affect the normal and functioning muscle cells of the affected limb.
This happened after a simple hematoma.
https://steemit.com/steemiteducation/@immarojas/have-you-ever-been-inside-a-cardiac-catheterisation-laboratory