She was a 24-year-old nurse who started feeling the pain four days before she presented to the clinic. Her jaw was a bit swollen, and she was in obvious distress. After taking a brief history, she explained that the pain was so severe it was causing headaches and interfering with her sleep; this prompted her to use pentazocine for the pain. I was shocked, as I expected her to use something as basic as ibuprofen or the regular diclofenac, and here is why:
Pentazocine belongs to the class of drugs known as narcotic analgesics (pain medicines). It relieves moderate to severe pain by acting on the brain. When a narcotic medication is used for an extended period, it can become addictive, resulting in mental or physical dependence.
I guess she understood this, being medical personnel herself, and presented at the clinic before she got addicted.
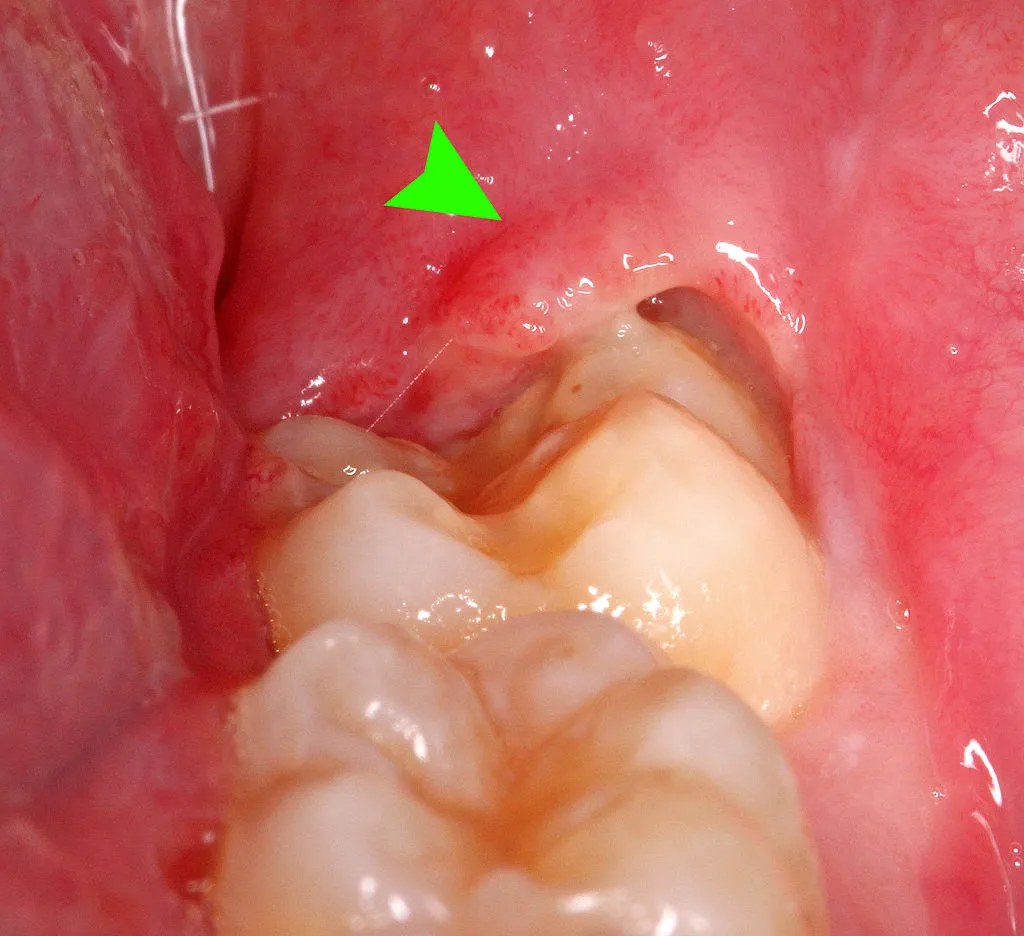
After a quick assessment, I discovered it was her last tooth on the lower jaw, but it had not fully erupted. I already had a diagnosis but proceeded to take an intra-oral radiograph that revealed tooth impaction.

Tooth impaction is when a tooth fails to erupt or is not completely erupted because the space available for the eruption path is insufficient or erupts in the wrong direction. It is commonly seen with wisdom teeth.
There are four forms or types of impaction; mesial-angular, vertical, horizontal, and distal-angular.
In mesial-angular impacts, the tooth is partially erupted and angled towards the front of the mouth. It is the most common type of impaction.
If there are horizontal impactions, the tooth lies entirely horizontally beneath the gums. In vertical impactions, the tooth is in the proper position for an eruption but remains below the gums.
Distal-angular impaction is the most uncommon type; the teeth are angled towards the back of the mouth and partially or completely impacted.
The radiograph confirmed my diagnosis: pericoronitis secondary to mesial-angular impaction of the wisdom tooth.
I explained the different management modalities; in her case, the best was to have Operculectomy Still, she opted for a surgical extraction because there was a higher chance of recurrence with operculectomy.
What exactly is pericoronitis?
Introduction
Pericoronitis is an intraoral inflammatory process caused by gingival tissue infection around or overlying an erupting or partially erupted tooth. Although it can occur with any erupting tooth, it is mostly associated with the eruption of the lower third molars (wisdom teeth).
About 75% of patients with pericoronitis have an operculum (flap of the gum tissue) partially covering the crown of the erupting tooth.
Causes and Risk Factors
It's commonly seen in people between 20 and 29 years of age. It is the period when most people are erupting their last molars.
Partially erupted lower 3rd molars are the major predisposing factors to developing pericoronitis. In addition, in some cases, poor oral hygiene and people with excess gum tissue are likely to have pericoronitis.
Types of Pericoronitis
Usually, it is classified based on the duration and severity of symptoms.
Whereas acute pericoronitis involves fever, severe pain, and swelling for one week, the symptoms of subacute pericoronitis are milder.
Pathophysiology
The space beneath the operculum is a stagnation area for food particles and debris, which now becomes a focus for infection by a mix of bacterial species found in the mouth, including streptococci and, in particular, various anaerobic species. It can then lead to abscess formation. If left untreated, the abscess beneath the operculum can spontaneously drain into the mouth.
Symptoms
Mostly, they present with severe pain around the wisdom tooth, rated 8 out of 10, and gum swelling. In some patients, you can see the imprint of the opposing tooth on the swelling.
Some patients experience bad breath due to abscess formation; there could be a discharging sinus from which pus discharges into the mouth. On rare occasions, some people might experience pain when swallowing and lockjaw.
Diagnosis and Investigations
It is a very easy condition to diagnose; you can be certain with a good history and proper clinical assessment. However, investigations such as intraoral radiographs are important to bolster the diagnosis and determine the modality of treatment.
Management
Several factors must be considered when treating pericoronitis, one of which is the duration of the condition, whether it is acute or subacute pericoronitis.
The major treatment modalities are to manage the pain using analgesics or local anesthesia (in some cases). When the gum flap is so wide it's covering the whole tooth, operculectomy (removal of the gum flap) is done. The downside of this is that there could be a recurrence.
A surgical extraction rather than an operculectomy will be done in patients with tooth impaction.
Most patients opt for this option because the recurrence rate of pericoronitis is almost zero.
In the case of subacute pericoronitis, home treatment can be done but not in place of professional care.
Some over-the-counter analgesics such as Ibuprofen, Diclofenac, and paracetamol can be used to alleviate the pain.
Good oral hygiene cannot be over-emphasized; regularly brushing and flossing is important to reduce the risk of food stagnation.
It would help if you did a warm saline mouth bath (warm water and salt rinse) or hydrogen peroxide rinse (1:4 dilution) at least three times daily. If you have a fever, do not use hot compresses; visit your dentist immediately.
Prognosis
The prognosis is good, with a 100% recovery rate if treated early. However, there could be complications.
Complications
Every condition has a complication, and pericoronitis is not any different. While most of these are rare, they occur if pericoronitis is left untreated.
One such example is space infections. It occurs when the infection tracks into the spaces present in the head and neck region.
While it is uncommon, a person suffering from pericoronitis can develop Ludwig's angina, a potentially fatal complication where the infection involves the submental, sublingual, and submandibular spaces.
A rare complication is bloodstream infection from the tooth, also known as sepsis.
Conclusion
Pericoronitis is a common condition that can be treated. My patient went home happy and satisfied.
References
WHO
CDC
Healthline