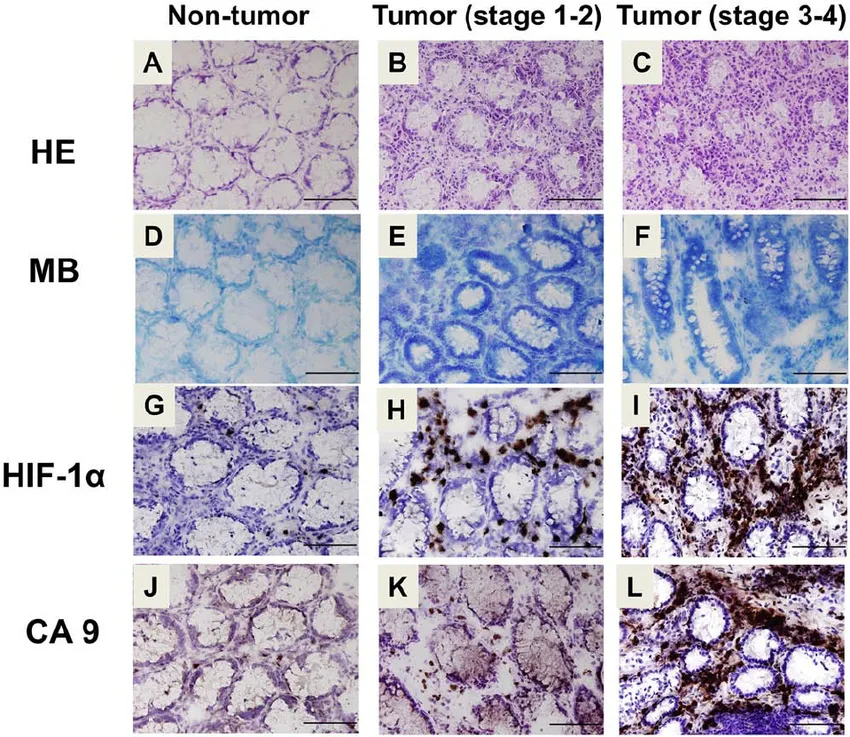
*Level of HIF-1a (an indicator of hypoxia) in healthy tissue compared to various states of tumor progression.
One of the questions I’ve been trying to develop an intellectually satisfying answer to for the past decade is: Why did Kwasniewski and Lutz seem to advise against ketosis, was it empirical or esoteric?
I find the hypoxic in utero environment of the fetus and subsequent metabolic transition of the neonate to a normoxic environment and eventual metabolic transformation fascinating. After gestation interesting things are occurring metabolically, increases in lactate, increases in ketogenesis and gluconeogenesis. The scant number of tracer studies looking at infant metabolism seem to indicate that exogenous lactose from breast milk and endogenous glucose as a result of gluconeogenesis is being shunted towards biosynthetic pathways and glucose is metabolically spared. In breast fed infants, glucose concentrations increase cyclically maintaining normoglycaemia. In contrast, infants administered oral solutions of glucose develop cyclical hypoglycemia.
I suspect there are morphological and functional differences between infant and adult mitochondria. There are reasons for this suspicion. Infants administered glucose less than 1 month after gestation present with glucose intolerance and glucose tolerance subsequently increases over the following months of development; additionally, the metabolic substrate profile points in that direction.
Infants have generous amounts of adipose tissue and as the infant transitions to a toddler and child, adipose tissue declines. I would suggest this is a result of maturing mitochondrial morphology and function; and that elevated lactate and ketones reflects fatty acid oxidation (FAO) capacity. This physiological metabolic transition is a result of adapting to an externally normoxic environment. Interestingly, for every 1000 meter increase in elevation there is a reduction in neonate mass and an increase in the incidence of fetal death.
One of the central tenets of my hypothesis is that ketone formation indicates hypoxia be it a histophysiological adaptation to external environmental conditions and physiological stimuli or; a pathophysiological disorder resulting from chronic exposure to compounds and energy substrates that interfere with or block normal histophysiological adaptations. In other words, anything that chronically interferes or blocks normal homeostatic processes produces a maladapted and eventually, unadaptive state, leading to entropy i.e. degeneration and death.
There is a beautiful cyclical metabolic signature from conception to death reflecting our ability to deal with oxygen and lack thereof; the energy substrates that build and prepare us for an oxygenated environment are eventually the same energy substrates that kill us. We develop in a hypoxic in utero environment and adapt to an oxygen rich environment. After birth and in the presence of oxygen our physiology matures and develops reflecting the external environmental conditions. As our mitochondria learn how to breathe, we slowly loose the ketogenic capacity present during early stages of life and transition to a reliance on fatty acids and develop the capacity to rely on glucose, fructose, and ketones when intermittent hypoxia is present. When intermittent hypoxia is present our mitochondria temporarily uncouple and become physiologically insulin sensitive and glucose is used to facilitate adaptation via biosynthetic pathways.
As we age our ketogenic capacity continues to decline along with a diminishing fatty acid oxidation capacity. In the context of this decline, not only do we lose the ability to produce adequate ketones to continually adapt to intermittent hypoxia, our mitochondria degenerate losing the ability to metabolize fatty acids and our physiology becomes more and more reliant on glucose as a metabolic substrate and as a result we lose the ability to maintain physiological insulin resistance. Slowly the adaptive state of intermittent physiological insulin sensitivity becomes pathophysiological and we lose the physiological insulin resistance of our youth.
As I have reflected on in the past, glucose is a primitive energy substrate, a glucose driven metabolism, contrasted with glucose used as a biosynthetic substrate in the context of a fatty acid driven metabolism, will drive primitive histophysiology and the subsequent degeneration of the orchestra. Every day the orchestra slowly goes out of tune and eventually the musicians slowly start disappearing, eventually the conductor has no musicians and he will turn to the audience, take a bow, and you will take your last breath.
In the end you will suffocate to death.
Why did Kwasniewski and Lutz seem to advise against ketosis?
- Whether they knew better or not, chronic ketosis indicates hypoxia.
- The conservative amount of glucose needed to stay out of deep chronic ketosis facilitates physiological insulin resistance and supports adaptive physiological insulin sensitivity during intermittent hypoxia.
- Ketosis reflects fatty acid oxidation capacity.