Hello,
I am going to try and put down my experience of the Continuing Health Care (CHC) process in England and the method I used to successfully secure CHC for my relative.
The reason I am referring to England only and not the UK is because different regions of the UK have slightly differing regulations.
Therefore my experience is with the English regulations.
Introduction
This is a very complex subject and this puts most people off claiming. It has been dramatised in a BBC TV Production called 'Care'.
The financial costs of ignoring this benefit can be significant considering Care Home residency costs of £770.00 per week, payable from the funds of the sick person. Any top up costs offered by the Care Home for additional niceties are the responsibility of Family members and not the sick person.
If NHS CHC is found to apply these payments are met by the NHS at no cost to the ill person. Top Ups are still the responsibility of Family Members.
Also you don't have to be in a Care Home to be eligable for CHC, the NHS is required to provide it's services at the point of need, so CHC can be applied for to pay for home visits and medical equipment at home.
There is a fast track system as well for those who are sadly nearing the end of their lives.
The ill person or their representative can apply for CHC, or if the patient has spent time in hospital and it is evident that they will not be able to live independalty, the hospital may complete the CHC Checklist on their behalf.
CHC Checklist
Initially the Claimant (ill person) needs to undergo a Checklist assessment before proceeding to a Multidisciplinary Team Meeting.
Lots of information can be found online regarding this by just searching online for CHC and Checklist.
If a patient is referred by a hospital the Checklist may be completed by the hospital and this stage may appear to have been skipped, as in our case.
CHC - Multidisciplinary Team Meeting
A Multidisciplinary Team Meeting is to assess a persons eligibility for NHS England CHC.
I found the term Multidisciplinary misleading personally as the disciplines it refers too are Social Services and Health Services, not Multiple medical disciplines such as Psychiatry, Urology etc.
A Decision Support Tool (DST) is filled in by the CHC Assessor (Medical lead) and the Social Worker. This document is almost always abreviated to the DST.
The aim of the meeting is to go through 12 'Domains', one by one and determine a persons rating in each of the twelve 'Domains'. The documents used list fixed statements of treatments for that 'Domain' with examples of gradually increasing degrees of medical complexity to determine a score for each 'Domain'.
My finding was these medical examples were interpreted very rigidly.
Taking the Continence 'Domain' as an example, the following details are listed:
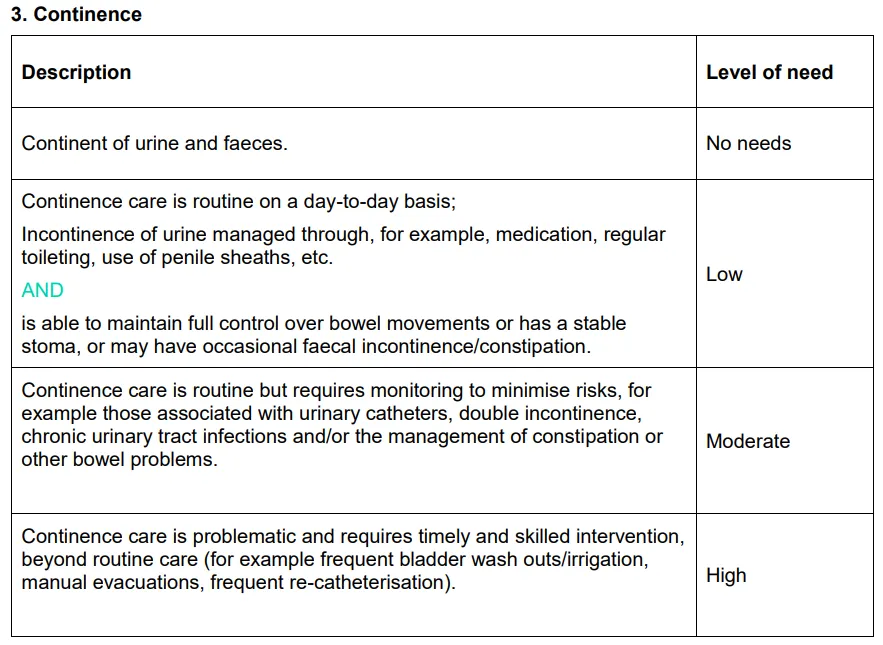
Source: UK Government
https://www.gov.uk/government/publications/nhs-continuing-healthcare-decision-support-tool
In this example if you are continent of Urine and Faeces you are No Needs, and you are only High needs if the given examples apply to you, and / or an equivalent. In one instance during the MDT we were told the requirement for a rating of High was someone who required regular medical procedures to remain continent. (ie puncturing of skin for catheta for example)
So what happens if the person has poor spatial awareness, forgets where the toilet is or walks head down without looking where they are going. They don't realise there is a light in the toilet and they don't use it, and go in the pitch black. Or they exhibit all four of these symptoms and are fully continent.
In some cases the Assessors are frugal with the facts and state no instances of incontinence of urine or feaces in the preceeding period. Yet the care records clearly show there has been many instances of both forms of incontinence.
The Family in question knew nothing of this in the Multidisciplinary Team Meeting as they were extremely naive and trusting of the process.
In my Families case we had to get hold of a copy of our relatives hand written Care Records and enter each comment as best we could into a spreadsheet. With hand written notes, this is not an easy or quick task.
In my opinion these facts combined with our interpretations was crucial to our success at Appeal.
The scores of each 'Domain' are then compared against a scoring mechanism to determine eligibility. So if you score well in Mobility Domain but poorly in the other 11 'Domains' you are very unlikely to be eligable.
If you are turned down there is an option to Appeal, but this tends to be on technicalities. In our case these technicalities were:
It was recorded that Family were consulted, but all of the Families comments were omitted in the documentation.
I was invited to submit my comments additionally by email (which took me 4 hours to compose) yet, this again was omitted.
One of the Carers at the Care Home left the meeting and another joined, this was not reflected in the list of attendees.
The meeting was dominated by The CHC Assessor and the Social Worker who is required to actively take part in the discussions was silent until the end of the meeting.
Again my view was that this meeting was run by a CHC Assessor who did not work for the NHS, the role seemed to have been contracted out.
It was also decided on Appeal that a 1 week period of observations was too short and this was increased to 4 weeks.
The twleve 'Domains' are as follows:
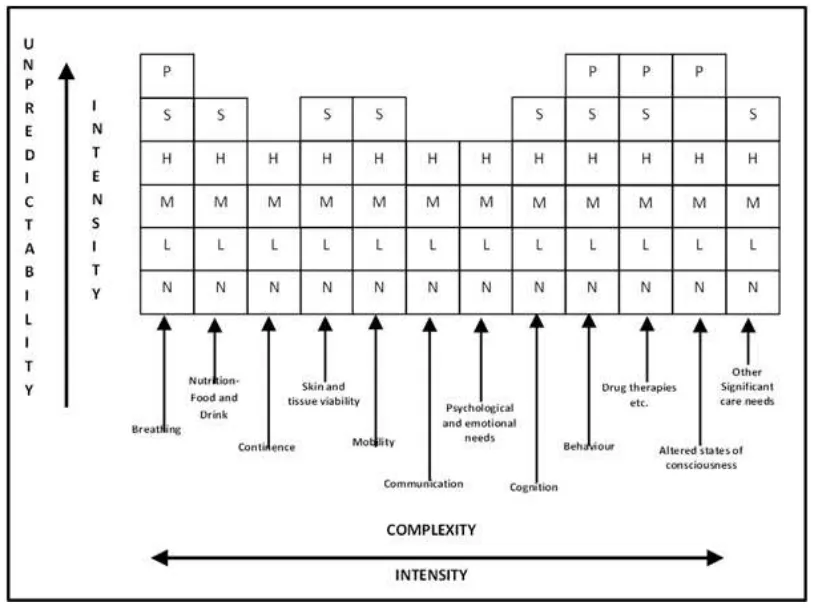
Source: UK Government
https://www.gov.uk/government/publications/nhs-continuing-healthcare-decision-support-tool
Horizontally all of the Domains are named and vertically going upwards there are letters.
The key for these letters are as follows:
N = No needs
L = Low needs
M = Medium needs
H = High needs
S = Severe need
P = Priority or threat to life need
All of the twelve Domains go up to High, only some go to Severe and only 4 to Priority.
To be eligable for NHS Continuing Healthcare you have to be deemed to have a Primary Health Need (PHN), the following scores will count as a PHN:
1 * Priority = success
2 * Severe = success
4 * High and 1 * Severe = success, however this seems to be purely discretional to the Multidisciplinary Team (MDT)
On the periphery of the chart are 3 very important words. In my opinion the 12 Domains are the smoke and mirrors put in place to distract you from Unpredicatbility, Intensity and Complexity, there is a fourth word (Nature) that is completley missing from the diagram.
Remember the Continence Domain example above, the Multidisciplinary Team Meeting guidance seemed to focus purely on Complexity of any medical intervention, yet Intensity and Unpredicatbility were barely mentioned.
These four words are given the name of the 'Key Indicators' or 'Characteristics'.
CHC Appeal
CHC has a rulebook that then NHS Trusts must follow when deciding on CHC eligability, these rules are you friends, then rulebook is called the National Framework, quote the National Framework paragraphs if you think it is warranted.
The National Framework consists of numbered paragraphs detailing each rule. It is in some of these paragraghs that the National Framework lists the technical reasons you can leverage to Appeal a decision.
This is how the National Framework described the Key Indicators or as thay have put it the Four Characteristics:
3.3 ’Nature’ is about the characteristics of both the individual’s needs and the interventions required to meet those needs.
Questions that may help to consider this include:
• How does the individual or the practitioner describe the needs (rather than the medical condition leading to them)? What adjectives do they use?
• What is the impact of the need on overall health and well-being?
• What types of interventions are required to meet the need?
• Is there particular knowledge/skill/training required to anticipate and address the need? Could anyone do it without specific training?
• Is the individual’s condition deteriorating/improving?
• What would happen if these needs were not met in a timely way?
3.4 ‘Intensity’ is about the quantity, severity and continuity of needs.
Questions that may help to consider this include:
• How severe is this need?
• How often is each intervention required?
• For how long is each intervention required?*
• How many carers/care workers are required at any one time to meet the needs?
• Does the care relate to needs over several domains?
3.5 ‘Complexity’ is about the level of skill/knowledge required to address an
individual need or the range of needs and the interface between two or more needs.
Questions that may help to consider this include:
• How difficult is it to manage the need(s)?
• How problematic is it to alleviate the needs and symptoms?
• Are the needs interrelated?
• Do they impact on each other to make the needs even more difficult to address?
• How much knowledge is required to address the need(s)?
• How much skill is required to address the need(s)?
• How does the individual’s response to their condition make it more difficult to provide appropriate support?
3.6 ‘Unpredictability’ is about the degree to which needs fluctuate and thereby
create challenges in managing them. It should be noted that the identification of unpredictable needs does not, of itself, make the needs ‘predictable’ (i.e. ‘predictably unpredictable’) and they should therefore be considered as part of this key indicator.
Questions that may help to consider this include:
• Is the individual or those who support him/her able to anticipate when the
need(s) might arise?
• Does the level of need often change? Does the level of support often have to
change at short notice?
• Is the condition unstable?
• What happens if the need isn’t addressed when it arises? How significant are
the consequences?
• To what extent is professional knowledge/skill required to respond
spontaneously and appropriately?
• What level of monitoring/review is required?
Source: UK Government
https://www.gov.uk/government/publications/national-framework-for-nhs-continuing-healthcare-and-nhs-funded-nursing-care
In another case a person was assessed to be Severely Cognitively Impaired in the Multidisciplinary Team Meeting, however in the Communication Domain this person was considered to have Medium needs. The DST itself states:
Unable to reliably communicate their needs at any time and in any way, even when all practicable steps to assist them have been taken. The individual has to have most of their needs anticipated because of their inability to communicate them.
It had to explained that a Severely Cognitively Impared person cannot comprehend their own needs to be able to Communicate them, therefore for the purposes of the DST the relative should automatically score High in the communication Domain as they were Unable to reliably communicate their needs at any time and in any way.
The key process I found to submit our case was to take each Carers statement from the Care records and highlight key information and then put notes underneath the statement explaining the reasoning.
The following example is purely fictitious...
30/04/22 12:00 - 13:00
As usual 'A' has been mobile throughout the day, distracted with treats to keep 'A' at the dining table. 'A' has been aggressive towards a member of staff, shouting and threatening them. 'A' stumbled and fell hurting their arm, a bandage was applied to the skin tear and the bleeding has now stopped. 'A' has become upset after wetting themselves during lunch but refuse personal care.
Nature:
Degenerative Undiagnosed Dementia (Dementia is diagnosed, the type (there are at least 3) is undiagnosed)
Desire to wander constantly during the day. (Symptom of Dementia)
Risk of dehydration, needs constant prompting to drink fluids and requires monitoring. (Dehydration is the main cause of death for Dementia sufferers)
Not able to concentrate on a task or activity.
Waterlo 11 (Waterlo is a medical method of recording skin thickness and likely hood of tearing), risk of skin tears
Gradual long term weight loss due to lack of appetite
Intensity:
Mobile throughout lunch, time consuming to keep having to bring 'A' back to the table to eat, can happen many times during one meal.
Complexity:
Nutrition Domain affected by Behaviour Domain.
Nutrition Domain affected by Mobility Domain.
Nutrition Domain affected by Skin Integrity Domain.
Nutrition Domain affected by Continence Domain.
Nutrition Domain affected by Psycholigical and Emotional needs Domain.
Domains interacting or overlapping make Complexity, multiple Domains interacting this way highlight a Primary Health Need.
Unpredicatbility:
'A' stumbled and fell hurting their arm. There is no previous medical history of falls mentioned in Nature. 'A' fell unpredictably, now falls risk will need to be taken into consideration.
Hopefully you will remember the Key Indicators or Characteristics of:
Nature
Complexity
Intensity
Unpredicatbility
The DST Form section for Nutrition is as follows:
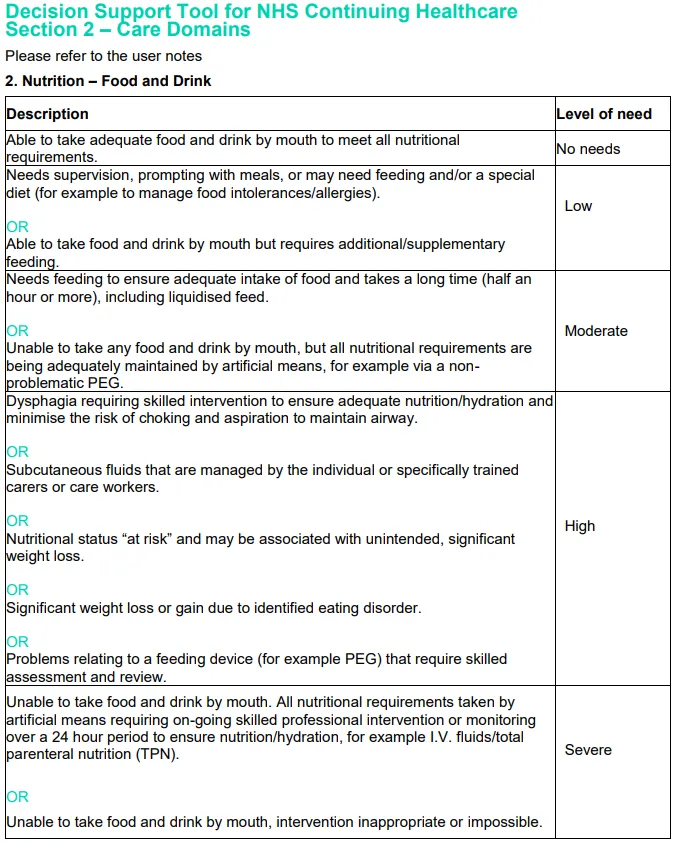
Source: UK Government
https://www.gov.uk/government/publications/nhs-continuing-healthcare-decision-support-tool
No Needs
As Nature does not mention problems with swallowing when eating and drinking then the Multidisciplinary Team (MDT) may decide No Needs applies.
Low Needs
If the CHC Assessor and the Social Worker are at odds and cannot agree which rating applies then the highest rating being considered should be used, so it is possible the MDT could decide on Low Needs.
Medium Needs
'Takes a long time (half an hour or more)'. As it is recorded in Nature that due to Wandering 'A' has to be brought back to the table to eat and 'A' struggles concentrating on tasks or activities it could be argued that meal times take longer than 30 minutes. In this instance Medium Needs may apply.
High Needs
Nature states that 'A' has 'gradual long term weight loss due to lack of appetite.' could fit 'Nutritional status at risk and may be associated with unintended, significant weight loss.' This could lead to a decision that High Needs applies.
Severe Needs
'Risk of dehydration, needs constant prompting to drink fluids and requires monitoring.' in Nature could fit with 'or monitoring over a 24 hour period to ensure Nutrition / hydration' could affect this decision and lead to a decision that Severe Needs applies.
The Decision Support Tool (DST) would lead you to believe the decision is about how medically complex a procedure is to be eligable, however it is the Four Key Indicators / Characteristics that are instrumental in being accepted for CHC.
Hopefully this example shows that the Four Characteristics, if used can present a more defined picture of 'A's needs and may effect the CHC decision.
Also don't be afraid to be wrong, the MDT will filter any mistakes you make and disregard them if they don't agree, however nothing ventured, nothing gained. A most of us aren't medical professionals.
I misunderstood Other Significant Care Needs and completely messed it up, it was explained that I had got it wrong and why it didn't apply as I thought it would.
Once CHC is awarded, it is not for life, there will be a re-assessment after 3 months and every twelve months thereafter.
As a closing note, I would like to say that not everybody will be eligable for CHC funding, but developing the above process saved my relative a whole heap of their lifes savings, but more importantly my relative also got better care through a better understanding of their needs.
If this article helps just one person with this subject I will be more than happy.
@onw - Splinterlands
@b8l - RisingStar
PS: I have been advised that because this article is not 100% original content (some text and pictures are taken from the UK.Gov website in an attempt to add context) I should at the very least decline rewards. I have opted to decline rewards when posting this hopefully final edit. (is there such a thing as Posting OCD?)
When I first posted, and subsequently edited, rewards were set to 50/50.