French neuroscientists have "awakened", in part, a 35-year-old man by stimulating a cranial nerve.
Will one day be able to awaken patients who have remained "unconscious" for several years? This is the mad hope of work published Monday, in the journal Current Biology. Researchers at the Institute of Cognitive Sciences Marc Jeannerod de Bron and the neurological hospital Pierre Wertheimer in Lyon have succeeded in passing a man immersed for fifteen years in a "vegetative state" to a "minimal state of consciousness" by stimulating a nerve connected to the brain.
To achieve this, the neurosurgeons of Lyon equipped this young patient of 35 years, victim of a road accident at 20 years, with a sort of "cerebral pacemaker". Installed at the level of the clavicle, it allows to stimulate the vagus nerve in the neck, a technique used for more than twenty years in the treatment of certain drug-resistant epilepsies. Recall that the vagus nerve connects the brain stem, located at the base of the brain, with the viscera (heart, lung, stomach, etc.). "It is this nerve that ensures so-called vegetative functions such as breathing, heart rhythm or digestion," explains Benjamin Rohaut, neurologist-resuscitator and researcher at Columbia University in New York. Physicians then sent electrical pulses for 30-second intervals of 5 minutes, day and night, for six months. Each week, the current intensity increased in steps to reach the maximum threshold of 1.5 mA (milliampere).
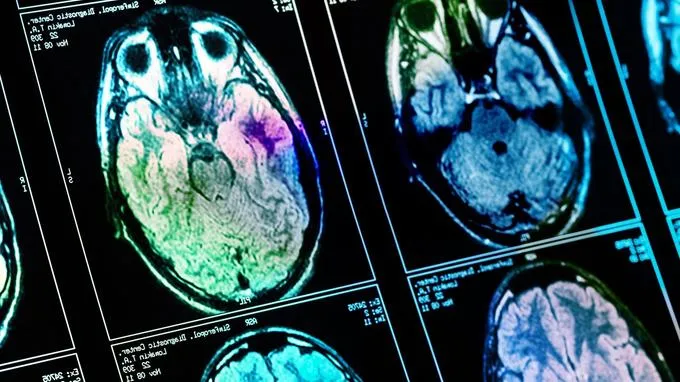
After a month, the neuroscientists found an improvement. "We have observed on the electroencephalogram the appearance of a wave which, according to recent works, seems to characterize the minimal state of consciousness, explains Angela Sirigu, director of research at the CNRS who supervised this project. And at the same time we measured an extension of the brain activity to areas that had not functioned for years. "Through the vagus nerve, researchers thought they had stimulated the brainstem, favoring re-ignition of nearby areas such as thalamus , which seems to play a key role in the state of consciousness. In 2007, deep stimulation of the thalamus, by inserting electrodes directly into the brain, yielded comparable results (the heaviness and dangerousness of the operation, however, never made it routine).
"These are very important jobs"
Clinically, the reactions of the patient are no longer limited to reflex activity. He is able to follow an object or a person's gaze, to turn his head on command and seems frightened when a face comes abruptly closer to him. Angela Sirigu tells that the young man would have shed two tears, a first spontaneous and a second to listen to his favorite song. "When asked to smile, he raises his left cheek," continues the researcher. "He has a real presence in his environment, he understands what he is told." Will that be enough to establish a communication system? "That's what we want. It's now up to the clinical team. "
"These are very important jobs," says Steven Laureys, a professor of neurology at the university and CHU in Liège, and head of the Giga Consciousness group, who has been experimenting with various techniques of "awakening" for several years. "This goes against the old dogma that one can not do anything for a patient after several years spent in such a state - which, in passing, should be called a" non-responding state of awakening "rather than of "vegetative state", a term too pejorative. "If this enthusiasm is widely shared, all neuroscientists also call for great caution. "This is a study of a single patient," warns Jacobo Sitt, an Inserm researcher at the Brain and Spinal Cord Institute in Paris. "This is a great achievement, but it is impossible to generalize it. Each patient is different. It is impossible to predict how much will be able to respond to this type of stimulation. All the lesions are not reversible. "Angela Sirigu has already begun recruiting for a new trial that should cover four patients, and could be extended to twenty if positive. The identification of the patients most likely to respond to this type of therapy would be ideal, but this would require extensive explorations using state-of-the-art brain imaging techniques.
The stimulation of the vagus nerve in this indication is only in its infancy
"Conceptually, it's very interesting," notes Andrea Rossetti, associate professor of neurology at the Lausanne Vaud University Hospital. "But it is almost certain that this patient will never regain his autonomy. Nor is he sure that he can communicate with the people around him. It has gone from level 5 to a level that oscillates between 8 and 10 on the 23 levels of the scale used to estimate the state of consciousness. It is certainly a small improvement, but we must not give false hopes to families who live with one of their loved ones this dramatic situation. "And there are many. In France, about 2,000 people would live in a similar state of "non-responding awakening".
"This new research is very exciting because it validates some of our theoretical models and offers new therapeutic perspectives, but they also pose real ethical questions," Benjamin Rohaut said. "Is the patient better in this state of minimal consciousness than in a vegetative state for which we suppose the absence of consciousness? Does not he feel more pain? Does not he suffer more from his situation? These are real questions. "To which it is still very difficult to answer. "Patients affected by a locked-in syndrome are not as unhappy as one imagines from the outside," recalls Jacobo Sitt. "And some recent research suggests that patients in a vegetative state may still feel pain."
The stimulation of the vagus nerve in this indication is still in its infancy. At least two other teams in China and the United States are experimenting with a non-invasive stimulation technique behind the ear. Other techniques, such as transcranial magnetic stimulation (which involves the creation of currents in the cortex via magnets) could support the stimulation of the vagus nerve to further improve the patient's state of consciousness. "We are gradually emerging from the therapeutic nihilism in which the community has shut itself up," says Laureys. We must not give false hopes to people, of course, but it is equally dangerous to cultivate a "false despair". "

Source: Le figaro