Let me be kind to say welcome to my blog again. Alright! So as we continue our neuro pathology series, I will be discussing Acute Disseminated Encephalomyelitis (ADEM). So let's quickly get into it.
First, we cannot really say what is the main cause but then there are some reasons or triggers for Acute Disseminated Encephalomyelitis (ADEM) which is regarded as an autoimmune disease that could be triggered via pathogens such as viruses such as infection from Measles mumps, and rubella or exposure to the MMR vaccine which could be rear. It can be triggered by Streptococcus beta haemolyticus and Mycoplasma pneumonia. It can also be a result of susceptible genes, and people who are young. If a person has been infected with a pathogen the immune system undergoes phagocytosis displaying the MHC2 complex where it exposes part of the pathogen on its surface where it is presented to the helper T-cell where the T-cell receptor interacts with the macrophage which is the antigen-presenting cell and then interacts with the antigen. The Helper T-cell starts to create more cells that identifies this pathogens. The problem can begin as the protein on the cell membrane of the pathogen and the protein in the myelin sheath are similar causing the T-cells to attack the myelin sheath thinking it is the pathogen known as Molecular mimicry.
The T-cell passes through the blood-brain barrier to the areas where the neuro tissues exist. There are proteins that are similar to the myelin sheath protein in the area and they begin to release cytokines INT-1, INT-6, TNF-alpha, and Interferon gamma, which causes inflamations. The INT-1, INT-6, TNF-alpha act on the endothelial cell allowing for white blood cells to travel to the area of the inflammation, as well as inform the blood vessels in this neurons to dillate causing more white blood cells to get into the area as well as causing the cells to be leaky or parfurated similar to inflammatory effects. This cytokines and trigger chemotaxis, and stimulate macrophages to the area where there is phagocytocis of the oligodendrocytes, the myelin sheaths, and the neurons leading to plaques in the neuron as a result of injuries. This is the cause of Acute Disseminated Encephalomyelitis (ADEM). Then B-cells starts to get into the the area to start producing antibodies such as the IgG antibodies which taggeds the oligodendrocytes causing the macrophages to phagocyte the oligodendrocytes as well as the brain neurons.
Clinically when there is an exposure to the pathogens, it reacts with the immune system which causes the release of cytokines which would act on the hypothalamus which triggers an increase in body temperature causing fever, headache and nausea. and it can lead to the inflammation of the 2nd cranial nerve affecting the visual pathway causing optic neuritis. The oligodendrocytes can be destroyed thereby affecting the nerves of Cranial nerve 12, Cranial nerve 5 (trigeminal nerve), 7th cranial nerve (facial nerve), and the nucleus ambigus. It can also lead to pseudobulba palsy as a result of a lesion in the corticobulbar tract causing a decrease in mastication, absent facial expressions, dysphagia and dysphonia, and disatria. It can also affect the injury of the brain center leading to encephalopathy, it can also cause an injury in the reticular formation which will affect the level of consciousness, ataxia, and seizure. This can also lead to injury of the spinal cord where it affects the dorsal column responsible for fine touch, proprioception, and discriminative touch. If the red tract is injured, it will cause lesions of the upper motor neurons causing weakness, it could also lead to decrease in pain, and touch. It can also affect the anterior gray horn causing a lower motor neuron lesion leading to a decrease hypotonia.
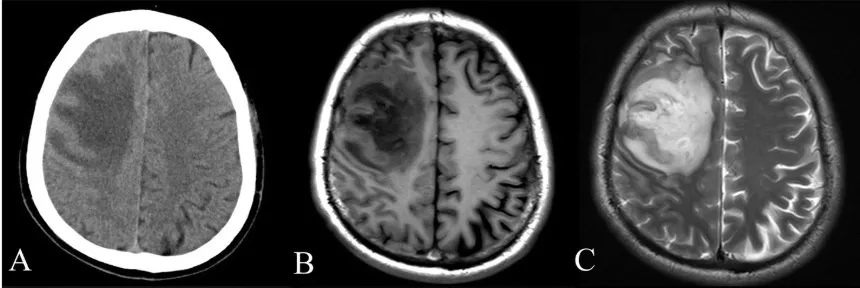
Diagnosing this condition has to do with an MRI of the brain and the spinal cord, showing lesions in the brainstem, cerebellum, and cortex. A lumber puncture can also be done to identify an increase in IgG antibodies, T-cells, macrophages, and increase in proteins. Treatment with start with high dose IV corticosteroid, Blood cleaning to eliminate the antibodies that are causing the inflamation (plasmapharacis),
IMAGE REFERENCE
Image 1 || Wikimedia Commons || CT and MRI scan of the brain with melioidosis
